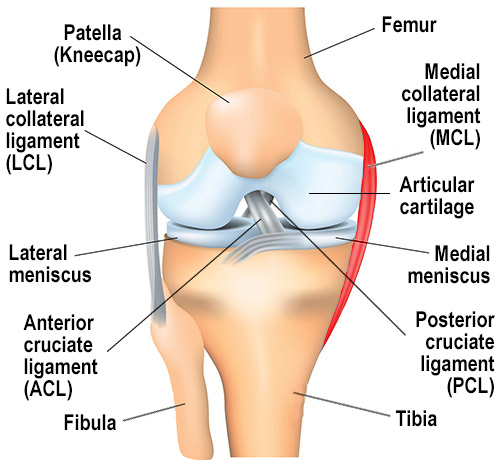
Have you ever wondered how the medial collateral ligament (MCL) stabilizes your knee? As one of the most critical ligaments in the knee joint, the MCL plays a vital role in preventing excessive valgus forces and ensuring joint stability. Understanding its anatomy is essential for both patients and medical professionals, as it directly impacts diagnosis, treatment, and recovery processes.
The MCL is a complex structure, and its anatomy is deeply studied in cadaveric research. For instance, a study involving 10 cadaveric human knees revealed significant details about the MCL’s insertion areas and measurements1. The mean age of the donors was 61.2 years, and the insertion area of the superficial MCL on the tibia was found to be 348.6 ± 42.8 mm², while on the femur, it was 79.7 ± 17.6 mm²1. These precise measurements highlight the importance of anatomical accuracy in surgical and therapeutic contexts.
Clinicians often emphasize the importance of understanding terms like collateral ligament and medial collateral in surgical planning. This knowledge helps in developing effective treatment strategies, especially for injuries involving the MCL and other ligaments like the LCL2.
Key Takeaways
- The MCL is crucial for knee stability and preventing valgus forces.
- Cadaveric studies provide detailed insights into MCL anatomy and measurements.
- Understanding MCL anatomy is vital for accurate diagnosis and treatment.
- The MCL works in conjunction with other ligaments like the LCL for joint stability.
- Precise anatomical knowledge aids in effective surgical and therapeutic strategies.
Introduction to Medial Knee Structures
The medial collateral ligament (MCL) is a cornerstone of knee stability, playing a pivotal role in preventing valgus forces and ensuring smooth joint function. As one of the knee’s key ligaments, the MCL is essential for maintaining structural integrity and enabling seamless movement.
Defining the Medial Collateral Ligament
The MCL is a robust ligament located on the medial (inner) aspect of the knee. It consists of two distinct components: the superficial MCL (sMCL) and the deep MCL (dMCL). The sMCL, with an average length of 94.8 mm, provides significant stability, particularly at 25 degrees of knee flexion, where it contributes 78% to joint stability3. The dMCL, while shorter, plays a crucial role in resisting valgus stress during various movements.
Importance in Knee Stability
Injuries to the MCL can significantly compromise knee mechanics, leading to functional deficits and increased risk of further damage. MCL injuries are the most common ligamentous knee injuries, accounting for 40% of all knee ligament injuries, with males being more prone than females4. These injuries often occur in high-contact sports like football and soccer, where direct blows to the lateral knee are frequent. The severity of MCL injuries is graded, with Grade I showing 3-5 mm of joint line opening, Grade II showing 6-10 mm, and Grade III exceeding 10 mm4.
Understanding the MCL’s components is vital for effective treatment and rehabilitation. The sMCL’s femoral attachment, located 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle, and its tibial attachment, 61.2 mm distal to the knee joint, highlight the precision needed in surgical interventions3. This anatomical accuracy is crucial for restoring joint stability and function, especially in cases where the MCL is injured alongside other structures like the ACL.
Understanding mcl knee anatomy
The medial collateral ligament (MCL) is a vital structure in the knee joint, providing stability and preventing excessive movement. Its anatomy is complex, with specific attachment points on the tibia and femur that are crucial for joint function.
The MCL consists of two layers: the superficial and deep layers. The superficial MCL is longer, with an average length of 94.8 mm, and provides most of the stability against valgus forces, especially at 25 degrees of knee flexion5. The deep MCL is shorter but plays a key role in resisting valgus stress during movement.
| Structure | Measurement | Contribution to Stability |
|---|---|---|
| Superficial MCL Length | 94.8 mm | 78% at 25° flexion |
| Tibial Attachment | 61.2 mm distal | Primary stability |
| Femoral Attachment | 3.2 mm proximal, 4.8 mm posterior | Structural integrity |
The MCL’s tibial and femoral attachments are precisely measured, with the tibial insertion area averaging 348.6 mm² and the femoral insertion at 79.7 mm²5. These measurements highlight the importance of anatomical accuracy in both treatment and understanding the ligament’s role in the knee joint.
In summary, the MCL’s structure and attachments are essential for knee stability. Understanding these details aids in effective treatment strategies and highlights the ligament’s crucial role in joint function.
Structure and Components of the MCL
The medial collateral ligament (MCL) is a complex structure composed of two distinct layers: the superficial MCL (sMCL) and the deep MCL (dMCL). Each layer plays a unique role in providing stability to the knee joint, particularly against valgus forces.
Superficial MCL Details
The superficial MCL is the longer of the two layers, with an average length of 100.7 mm. It is primarily responsible for resisting valgus stress, especially at 25 degrees of knee flexion, where it contributes significantly to joint stability1. The sMCL attaches proximally to the medial epicondyle of the femur and distally to the medial aspect of the tibia, approximately 61.2 mm distal to the joint line1. This broad attachment provides a wide base for stability.
Studies have shown that the insertion area of the sMCL on the tibia is 348.6 ± 42.8 mm², while on the femur, it is 79.7 ± 17.6 mm²1. These measurements highlight the importance of precise anatomical knowledge in surgical and therapeutic contexts.
Deep MCL Insights
The deep MCL, though shorter, is crucial for resisting valgus stress during movement. It is composed of two parts: the meniscofemoral ligament (MFL) and the meniscotibial ligament (MTL). The MFL is approximately three times longer than the MTL, while the MTL is about 1.7 times wider than the MFL1.
The deep MCL’s attachments are closer to the joint line, with the tibial insertion centroid located just 6.5 ± 1.3 mm from the tibial joint line1. This proximity allows the dMCL to provide additional stability and support to the knee joint.
Understanding the distinct roles and structures of both the superficial and deep MCL is essential for effective treatment strategies. Accurate repair of these components is critical in restoring knee function and preventing further injury.
Function and Biomechanics of the MCL
The medial collateral ligament (MCL) plays a crucial role in maintaining knee stability, particularly against valgus forces. Its biomechanical functions are essential for both static and dynamic support, ensuring proper joint function during various activities.
Role in Valgus Stress Restraint
The MCL is the primary stabilizer against valgus stress, especially at 25 degrees of knee flexion, where it contributes significantly to joint stability6. This ligament is also vital in protecting the leg during dynamic activities, preventing excessive movement that could lead to injury.
Dynamic Support During Movement
During movement, the MCL works in conjunction with the meniscus to maintain joint integrity. The ligament distributes stress across the knee, ensuring even load distribution and preventing overload on any single structure6. This anatomical and functional interplay is crucial for stability during various activities.
The MCL’s ability to resist valgus stress and provide dynamic support is vital for knee function. Understanding its biomechanics aids in developing effective treatment strategies and highlights its importance in maintaining leg stability and preventing injury.
MCL Anatomy in Total Knee Arthroplasty
Understanding the anatomy of the medial collateral ligament (MCL) is crucial for successful total knee arthroplasty (TKA). The MCL plays a significant role in maintaining knee stability, and its precise anatomical structure directly impacts surgical outcomes.
Implications for Soft Tissue Balancing
During TKA, preserving the integrity of the MCL is essential for proper soft tissue balancing. Studies have shown that the MCL contributes 57% of medial stability at 5 degrees of knee flexion and 78% at 25 degrees7. This highlights the importance of anatomical accuracy during surgery.
The release of the MCL, when necessary, must be done carefully to avoid instability. Research indicates that loss of MCL integrity can lead to significant instability, potentially affecting surgical results8. The correlation between joint line elevation and quadriceps peak force further emphasizes the need for precise tissue management9.
Preserving the natural tissue structure is vital for optimal outcomes. Integrating quantitative anatomical analysis into surgical planning can enhance results, though current data on MCL injuries in TKA is limited, underscoring the need for further research8.
In conclusion, understanding the MCL’s role in TKA is essential for achieving balanced soft tissue and stability, ultimately leading to better surgical outcomes.
Quantitative Morphological Analysis
Understanding the precise structure of the medial collateral ligament (MCL) is essential for both diagnosis and treatment. Recent studies utilizing 3D digitizing techniques have provided detailed insights into the ligament’s morphology, revealing critical measurements that aid in assessing function and injury risks.
Insertion Areas and Ligament Length Measurements
- The superficial MCL’s tibial insertion area measures 348.6 ± 42.8 mm², while the femoral insertion is 79.7 ± 17.6 mm²10.
- The deep MCL’s tibial and femoral insertion areas are 63.6 ± 13.4 mm² and 71.9 ± 14.8 mm², respectively10.
- The average length of the superficial MCL is 100.7 ± 9.5 mm, providing significant stability against valgus forces10.
3D Digitizing Technique Overview
3D digitizing offers high-precision data, crucial for analyzing ligament function and injury risks. This method highlights how measured forces correlate with injury likelihood, especially when comparing the MCL to cruciate ligaments11.
Such precise measurements are vital for advancing treatment approaches, ensuring accurate surgical interventions and rehabilitation strategies.
MCL Injury and Its Clinical Implications
Injuries to the medial collateral ligament (MCL) present unique clinical challenges due to their varying patterns and severity. These injuries are the most common among knee ligament injuries, often resulting from direct blows or sudden directional changes that produce valgus forces12. Understanding the implications of these injuries is crucial for effective diagnosis and treatment.
Common Injury Patterns
MCL injuries can range from partial to complete tears. Partial tears may allow for nonoperative management, while complete tears often require surgical intervention13. Injuries frequently occur when the knee is flexed at 20–30°, as this is when the superficial MCL is taut and most vulnerable13.
Diagnostic Challenges
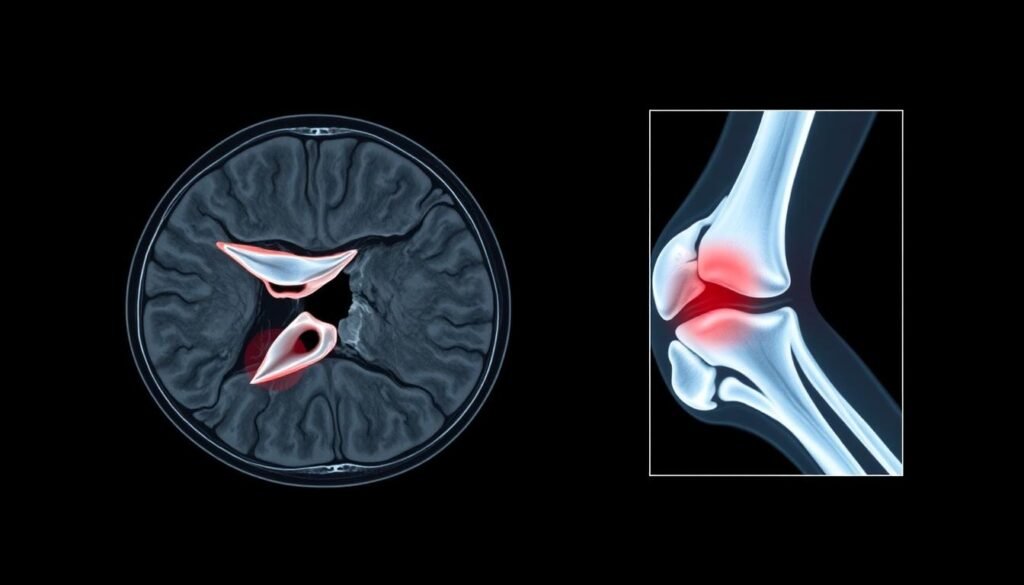
Diagnosing MCL injuries can be complex due to overlapping symptoms with other ligament injuries, particularly those involving the anterior cruciate ligament (ACL)12. Stress radiography and MRI are commonly used for diagnosis, with MRI being the gold standard for assessing ligament injuries12. Musculoskeletal ultrasonography (MSK-US) has also emerged as a reliable, cost-effective method for evaluating MCL injuries12.
For more detailed information on diagnostic techniques, visit our resource on clinical implications of MCL injuries.
Precise diagnosis is essential for guiding treatment strategies, whether through conservative management or surgical intervention. Accurate identification of injury severity ensures optimal outcomes, minimizing the risk of further complications.
Conservative and Surgical Treatment Options
When dealing with medial collateral ligament injuries, treatment options vary based on the severity and specific circumstances of the injury. Both conservative and surgical approaches have their place, each offering distinct benefits depending on the patient’s needs.
Non-Operative Management Strategies
For less severe injuries, non-operative management is often the preferred approach. This typically involves bracing, physical therapy, and gradual rehabilitation. Studies show that most people with MCL tears recover well with non-surgical treatment due to the ligament’s good blood supply14.
- Bracing: Provides stability and support during the healing process.
- Physical Therapy: Focuses on restoring strength and range of motion.
- RICE Method: Rest, Ice, Compression, and Elevation are initial steps to reduce swelling and pain.
Operative Repair Techniques
In cases where instability is significant or conservative treatment fails, surgical intervention is necessary. Operative techniques are compared to those used in cruciate ligament repairs, ensuring optimal results.
- Surgical Repair: Often required for complete tears or severe instability.
- Reconstruction: May be necessary for complex cases, especially when other ligaments are involved.
Statistical data highlights that return to sports varies with injury grade. Grade I injuries may see a return in 11 days, while Grade III injuries could take around 9.2 weeks15. Surgical failure rates are lower for reconstructions (4%) compared to repairs (20%)15.
Current articles emphasize the importance of tailored treatment plans, supported by studies showing 74% of patients achieving favorable outcomes with reconstruction15. This underscores the need for precise diagnostic techniques and personalized approaches in managing MCL injuries.
Imaging and Diagnostic Considerations
Imaging studies play a pivotal role in diagnosing medial collateral ligament injuries, offering insights into soft tissue integrity and joint stability. These diagnostic tools are essential for accurately assessing the extent of damage and guiding treatment plans.
MRI and X-Ray Findings
Magnetic Resonance Imaging (MRI) and X-ray are the primary imaging modalities used to evaluate MCL injuries. MRI provides detailed visualization of both the ligament and surrounding soft tissues, making it particularly effective in identifying partial or complete tears. X-ray, especially stress radiography, is valuable for assessing joint alignment and stability under load.
- MRI sensitivity in detecting MCL lesions is higher compared to clinical examination, though it may underestimate the severity of instability in up to 21% of cases16.
- Stress radiography demonstrates high specificity (100%) and sensitivity (93%) in identifying MCL injuries, with a positive predictive value of 1.0016.
| Imaging Modality | Sensitivity | Specificity |
|---|---|---|
| MRI | Varies widely (7% to 100%) | 40% to 100% |
| Stress Radiography | 93% | 100% |
These imaging techniques not only aid in diagnosis but also in monitoring the progress of injury repair and treatment effectiveness. Clinical examples from the literature highlight how precise imaging correlates with surgical findings, ensuring accurate diagnostic approaches.
Rehabilitation and Recovery Protocols
Rehabilitation after an MCL injury is crucial for restoring function and strength. Tailored exercises focus on areas like the side knee, while protecting the tibial plateau and femur.
Post-Treatment Knee Exercises
We recommend specific exercises to restore strength around the side knee. These include quadriceps settings and heel slides, which are gentle on the tibial plateau.
- Phase 1 lasts about 6 weeks for severe injuries and 3 weeks for mild ones17.
- A short-hinged brace is used for 3-6 weeks to support the side knee during healing.
- Ice application (20 minutes, 3 times daily) helps control pain and swelling.
| Exercise | Frequency | Details |
|---|---|---|
| Quadriceps Setting | 1-2 sets | 15-20 repetitions |
| Heel Slides | 1 set | 5-15 minutes with towel assist |
| Partial Squats | 3 sets | 15 repetitions, avoiding pain |
Gradual progression is key. Each portion of the protocol is monitored to ensure proper healing. Strengthening exercises for the side knee and surrounding structures are introduced in later phases, focusing on the femur and tibial plateau17.
Conclusion
In conclusion, our comprehensive study of the medial collateral ligament (MCL) highlights its critical role in knee stability and function. The MCL, working in tandem with structures like the posterior cruciate ligament, ensures joint integrity and movement. Understanding every aspect of the ligament, from its attachment at the epicondyle to its interaction with the pes anserinus, is vital for both diagnosis and treatment18.
Accurate measurements and timely treatment are essential for successful outcomes. Quantitative data, such as the 92% MRI grading agreement with clinical findings, informs both conservative and surgical approaches19. This data underscores the importance of personalized treatment plans, whether through nonoperative management or surgical intervention.
We encourage clinicians and researchers to integrate these insights into their practice and studies. By doing so, they can enhance treatment efficacy and improve patient outcomes, ensuring the MCL’s role in knee stability is fully leveraged for optimal results.
