Have you ever wondered how the medial knee structure impacts your mobility and stability? The medial knee, a complex system of ligaments and attachments, plays a crucial role in joint function and movement. Understanding its anatomy is essential for preventing injuries and ensuring proper healing.
The medial knee consists of the superficial medial collateral ligament (sMCL), deep medial collateral ligament (dMCL), and posterior oblique ligament (POL). These ligaments work together to provide stability and prevent excessive motion, especially during activities like running or twisting. Injuries to these ligaments can significantly alter joint biomechanics and lead to conditions like medial compartment gapping.
Recent studies show that medial knee injuries are the most common type of knee injury, with the sMCL being the most frequently damaged stabilizer in sporting injuries1. A simulated grade III sMCL injury can increase medial compartment gapping by 3.2 mm compared to the intact state2. This highlights the importance of proper diagnosis and treatment, as even minor lesions can have significant effects on joint stability.
Key Takeaways
- The medial knee structure includes the sMCL, dMCL, and POL, which are crucial for joint stability.
- Medial knee injuries are the most common type of knee injury, often involving the sMCL.
- Grade III sMCL injuries can lead to significant medial compartment gapping, affecting joint function.
- Proper diagnosis and treatment are essential to prevent long-term damage and restore mobility.
For more information on the medial compartment of the knee, visit our detailed guide: Medial Compartment of the Knee.
Overview of the Medial Knee Structure
The medial knee structure is a vital component of our musculoskeletal system, playing a central role in movement and stability. Its intricate design ensures that we can perform daily activities like walking and standing with ease. This complex system is fundamental to our mobility and overall joint health.
Purpose and Importance
The primary role of the medial knee structure is to provide stability and support during various movements. It achieves this through a network of ligaments and attachments that work together to absorb forces and distribute weight evenly. Understanding this system is crucial for both preventing injuries and ensuring proper healing.
Role in Knee Stability and Function
The collateral ligament is key in resisting abnormal movements, such as valgus stress, which can occur during activities like running or twisting2. Specific attachment points along the tibia and knee joint line are essential for weight distribution and proper joint movement. Anatomical features play a significant role in diagnosing injuries and ensuring effective treatment.
| Component | Function | Importance |
|---|---|---|
| Collateral Ligament | Resists valgus stress | Prevents excessive joint movement |
| Tibial Attachments | Distributes weight | Ensures even load distribution |
| Knee Joint Line | Supports joint movement | Facilitates smooth motion |
Anatomical Components and Attachments
The knee joint is a complex system with precise anatomical components that ensure stability and movement. Understanding these elements is crucial for diagnosing injuries and developing effective treatments.
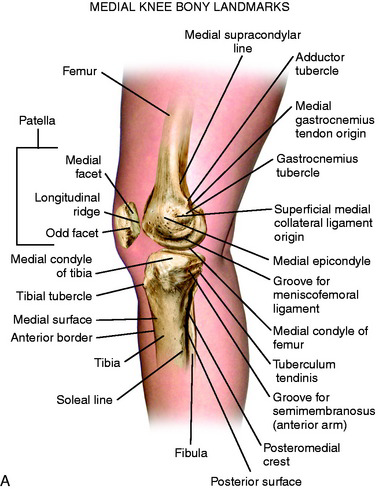
Osseous Landmarks and Attachment Sites
The medial knee features key bony landmarks, including the medial epicondyle and adductor tubercle, which serve as attachment points for ligaments and tendons. These sites are meticulously mapped using advanced tracking systems to understand their roles in joint stability3.
Studies highlight how these landmarks contribute to load distribution and rotation, ensuring smooth knee function. Accurate mapping of these areas is vital for both injury prevention and treatment4.
| Component | Function | Importance |
|---|---|---|
| Medial Epicondyle | Ligament and tendon attachment | Provides stability during movement |
| Adductor Tubercle | Muscle insertion point | Supports joint integrity |
| Gastrocnemius Tubercle | Tendon attachment | Aids in knee flexion |
Ligamentous and Tendinous Contributions
Ligaments and tendons work together to provide stability and facilitate movement. The collateral ligaments, for instance, prevent excessive joint movement, while tendons enable muscle forces to act on the bones.
Understanding the relationships between these tissues is essential for addressing injuries and restoring function. This knowledge also lays the groundwork for discussing ligament and tendon differences in later sections.
Deep Dive into the Medial Knee Structure
Understanding the layers of the medial knee is crucial for effective diagnosis and treatment. This complex system consists of both superficial and deep elements, each playing a unique role in joint stability and movement. These components work together to absorb forces and distribute weight, ensuring smooth function.
Superficial vs Deep Elements
The superficial elements, such as the sMCL, are more prone to injuries during activities like running or twisting3. In contrast, deep elements, including the dMCL and POL, provide additional stability and resist excessive motion. This distinction is vital for understanding injury patterns and developing effective treatments.
Injuries can selectively affect either superficial or deep structures, leading to different tear patterns. For instance, a grade III sMCL injury can increase medial compartment gapping by 3.2 mm5. This highlights the importance of proper diagnosis and treatment to restore joint function and prevent long-term damage.
Forces such as rotation impact each element differently, with superficial ligaments more susceptible to valgus stress. Muscle support and motion dynamics are interwoven with ligament function, ensuring proper joint movement. Clinical insights into these layers guide both conservative and surgical treatments, optimizing recovery outcomes.
Understanding the Medial Collateral Ligament (MCL)
The medial collateral ligament (MCL) is a crucial component of the knee, providing stability and resisting valgus stress. Its unique anatomy and function make it vital for both preventing injuries and ensuring proper healing. The MCL consists of both superficial and deep components, each playing a distinct role in joint stability.
Femoral and Tibial Attachments
The MCL attaches to the femur near the adductor tubercle and medial epicondyle, while its tibial insertion is located just below the joint line. These precise attachment points are essential for distributing forces evenly and preventing excessive joint movement. Studies have shown that valgus stress is the most common mechanism of injury for MCL tears6.
Superficial and Deep Components
The superficial MCL is more prone to injuries during activities like running or twisting, while the deep component provides additional stability. Injuries can selectively affect either layer, leading to different tear patterns. For instance, a grade III MCL injury can increase medial compartment gapping by 3.2 mm compared to the intact state7.
The MCL’s ability to absorb forces and distribute weight is critical for knee function. Tear patterns can significantly impact load distribution and joint stability. Understanding both tendon and capsule integrations with the MCL is essential for addressing injuries and restoring function.
| Component | Function | Importance |
|---|---|---|
| Superficial MCL | Resists valgus stress | Prevents excessive joint movement |
| Deep MCL | Provides additional stability | Resists rotational forces |
| Femoral Attachment | Distributes weight | Ensures even load distribution |
In conclusion, the MCL’s anatomy and function are central to knee stability. Proper diagnosis and treatment are essential to prevent long-term damage and restore mobility. This understanding sets the framework for discussing supporting structures and subsequent rehabilitation or surgical strategies.
Meniscus, Joint Capsule, and Other Supporting Structures
The meniscus and joint capsule play vital roles in knee joint stability and movement. These components work together to absorb shock and distribute loads, ensuring smooth function.
Medial Meniscus and Articular Cartilage
The medial meniscus covers about 60% of the tibial plateau, acting as a crucial load absorber8. It works closely with the articular cartilage to maintain smooth joint motion. The medial meniscus is fixed to the joint capsule and ligaments, making it more prone to injury when these structures are damaged9.
Pes Anserine Bursa and Muscle Insertion Points
The pes anserine bursa reduces friction between muscles and bone, particularly around the sartorius, gracilis, and semitendinosus muscles. This bursa is essential for preventing inflammation and ensuring smooth muscle function near the knee joint10.
| Component | Function | Importance |
|---|---|---|
| Medial Meniscus | Load absorption | Vital for joint stability |
| Joint Capsule | Supports joint movement | Ensures smooth motion |
| Pes Anserine Bursa | Reduces friction | Prevents inflammation |
These structures are integral to knee function, and their integrity is key to preventing injuries and ensuring effective treatment strategies.
Biomechanics and Load-Sharing Relationships
The biomechanics of the medial knee involve an intricate balance of forces and ligament interactions. This complex system works to distribute valgus and rotational forces efficiently, ensuring joint stability and movement.
Valgus and Rotational Force Resistance
Valgus forces are primarily resisted by the superficial medial collateral ligament (sMCL) across all ranges of motion, especially at 30º of flexion2. The deep medial collateral ligament (dMCL) acts as a secondary restraint to valgus forces, while the posterior oblique ligament (POL) resists rotational forces, particularly near extension2.
Functional Unit Interaction
Muscle coordination is crucial for maintaining balance during dynamic knee motion. Forces acting on the knee are redistributed to prevent overload, with anatomical landmarks like the adductor tubercle anchoring these forces11. This load-sharing relationship protects the knee in high-impact scenarios and informs both conservative and surgical treatments.
| Component | Function | Importance |
|---|---|---|
| sMCL | Resists valgus stress | Primary stabilizer against valgus forces |
| dMCL | Secondary restraint to valgus | Supports sMCL in stability |
| POL | Resists rotational forces | Key in preventing rotational instability |
This holistic view of biomechanics guides effective treatment approaches, ensuring optimal recovery and stability.
Common Injury Mechanisms and Their Impact
Understanding how injuries occur is crucial for prevention and treatment. Traumatic forces and repetitive overload often lead to more than just isolated tears, frequently causing damage to multiple ligaments within the medial knee unit12.
Traumatic Forces and Overload
Traumatic forces, such as twisting and pivoting, are common causes of medial knee injuries. These movements can lead to valgus stress and rotational forces, which often result in ligament tears. For instance, a blow to the outer side of the knee can cause an MCL injury, while a sudden pivot might lead to an ACL tear13.
Multi-Ligament Involvement
When one ligament is injured, it can create a cascade effect, impacting adjacent ligaments and tendons. This multi-ligament involvement is common in high-energy traumas, such as car accidents or severe falls, and can significantly compromise the knee’s stability12.
| Force Type | Common Injuries | Impact |
|---|---|---|
| Valgus Stress | MCL Tears | Compromised medial stability |
| Rotational Forces | ACL Tears | Joint instability |
| Direct Blows | PCL Injuries | Posterior instability |
Accurate understanding of these injury mechanisms is vital for developing targeted treatment strategies and rehabilitation plans.
Diagnosis and Imaging Techniques
Accurate diagnosis of medial knee injuries requires a combination of clinical examinations and advanced imaging techniques. These methods help identify the severity of ligament damage and guide effective treatment plans.
Clinical Examination and Assessment
Clinicians assess medial knee stability through specific stress tests and valgus load evaluations. These tests help determine the extent of injury and differentiate between isolated ligament damage and multi-ligament involvement14.
Subtle differences in ligament and tendon integrity are crucial for an accurate diagnosis. Stress radiography has shown high reliability, with a sensitivity of 93% and specificity of 100% in detecting MCL lesions15.
Utilizing MRI and X-Ray Evaluations
MRI is the gold standard for visualizing soft tissues, providing detailed images of ligaments and tendons. It highlights abnormalities that might not be visible on X-rays, improving diagnostic accuracy by 30-40%16.
X-rays are essential for assessing bony landmarks like the femoral attachment and adductor tubercle. They help quantify joint space opening under valgus stress, with a defined upper limit of 2.0 mm for true positive cases15.
| Imaging Modality | Key Features | Diagnostic Value |
|---|---|---|
| MRI | High-resolution images of soft tissues | Excellent for detecting ligament and tendon injuries |
| X-Ray | Assesses bony structures and joint alignment | Valuable for quantifying joint space changes |
| Stress Radiography | Measures joint space under stress | High sensitivity and specificity for MCL injuries |

Combining clinical assessments with imaging techniques ensures precise diagnosis, which is critical for developing effective treatment strategies for medial knee injuries.
Conservative Treatment and Rehabilitation Strategies
For many individuals with medial knee injuries, conservative treatment offers an effective path to recovery. This approach focuses on reducing pain, restoring strength, and improving joint stability without surgical intervention.
RICE Protocol and Physical Therapy
The RICE protocol—Rest, Ice, Compression, and Elevation—is often the first step in managing injuries. It helps minimize swelling and pain, especially in the initial stages17. Physical therapy plays a crucial role in the rehabilitation process, emphasizing exercises that strengthen the muscles around the knee, improving joint stability, and enhancing flexibility.
Patient-Specific Activity Modifications
Activity modifications are tailored to each patient’s needs to avoid overloading the injured structures. This might include avoiding certain movements or using supportive devices. Monitoring progress through stress tests and motion evaluations ensures the treatment plan is effective and adjustments are made as needed.
Studies show that 98% of athletes with grade I and II MCL injuries successfully return to play within 10 to 14 days using conservative methods17. However, grade III injuries may require more intensive interventions, potentially including surgery, especially in athletes to address rotational instability.
Conservative measures not only restore proper alignment and load distribution but also help prevent chronic issues like joint laxity and early osteoarthritis. This non-surgical approach is particularly beneficial for patients seeking to avoid the risks associated with surgery.
Surgical Interventions and Reconstruction Approaches
Surgical interventions for medial knee injuries are considered when conservative treatments fail to restore stability and function. These procedures aim to repair or reconstruct damaged ligaments, ensuring proper joint mechanics and preventing long-term instability.
Repair Versus Reconstruction Options
Deciding between ligament repair and reconstruction depends on the injury’s severity and chronicity. Repair is often preferred for acute injuries, as it preserves the native tissue and promotes faster healing18. However, reconstruction is typically recommended for chronic cases or when the ligament is severely damaged, ensuring long-term stability and function.
Considerations for Acute Versus Chronic Injuries
Acute injuries benefit from immediate surgical intervention to restore anatomy and prevent further damage. Chronic cases, however, require a more tailored approach, often involving reconstruction to address prolonged instability. Studies show that anatomical restoration is crucial for both scenarios, especially in restoring the femoral attachment and ligament anatomy19.
Optimizing Joint Function Through Reconstruction
Collateral ligament reconstruction techniques have evolved to optimize joint function. By restoring proper femoral attachments and ligament anatomy, these procedures significantly reduce medial compartment gapping. For instance, reconstruction of the sMCL and POL using a single femoral tunnel has shown a 98% success rate in restoring stability, with patients achieving IKDC scores of A or B19.
Key Considerations for Surgical Decisions
- Immediate surgery is often necessary for acute injuries to prevent chronic instability.
- Chronic cases may require reconstruction to address prolonged instability.
- Restoring femoral attachments and ligament anatomy is vital for long-term function.
- Reconstruction techniques can significantly reduce medial compartment gapping and improve joint stability.
These surgical approaches, supported by studies, highlight the importance of precise anatomical restoration in achieving optimal outcomes for patients with medial knee injuries.
Future Research and Evolving Clinical Perspectives
Recent advancements in understanding the medial knee’s complex interactions are paving the way for improved treatments and better patient outcomes. Researchers are focusing on how biomechanical insights can optimize ligament repair techniques and enhance diagnostic accuracy.
Emerging Evidence and Biomechanical Insights
Studies are uncovering the critical role of deep medial structures and the joint capsule in knee stability. For instance, the semimembranosus muscle is gaining attention for its load-sharing capabilities, which could revolutionize how we approach ligament reconstruction20.
Advancements in imaging technologies are also transforming treatment paradigms. High-resolution MRI and stress radiography are now providing clearer insights into ligament integrity, enabling more precise diagnoses and treatment plans21.
| Research Focus | Key Findings | Impact on Treatment |
|---|---|---|
| Deep Medial Structures | Increased emphasis on capsule contributions | Improved surgical reconstruction techniques |
| Semimembranosus Role | Load-sharing capabilities identified | Enhanced rehabilitation strategies |
| Advanced Imaging | Higher diagnostic accuracy | More personalized treatment plans |
These developments highlight the importance of continued research in refining clinical practices. By focusing on both biomechanical optimization and patient-specific care, future studies aim to significantly improve outcomes for those with medial knee injuries.
Conclusion
In conclusion, the complexity of the medial knee and its components underscores the importance of comprehensive understanding for effective diagnosis and treatment. Each ligament, muscle, and attachment plays a unique role in joint stability and function, as highlighted by studies showing the superficial medial collateral ligament (sMCL) is centered 4.8 mm posterior and 3.2 mm proximal to the medial epicondyle22.
Both conservative and surgical approaches are crucial, with conservative methods often resolving injuries in 10-14 days for grade I and II cases23. Surgical interventions, like sMCL reconstruction, restore stability with a 98% success rate23. Research continues to refine treatments, emphasizing anatomical restoration for optimal outcomes.
Future studies should focus on deep medial structures and advanced imaging to enhance diagnostic accuracy. Clinicians and patients must adopt a comprehensive approach to prevent chronic issues and improve knee health. By integrating biomechanical insights and patient-specific care, we aim to advance understanding and outcomes in knee health.
