Every year, over 1 million Americans face knee injuries that disrupt work, sports, and daily life. While many focus on quick fixes, the real challenge lies in matching injuries to precise treatments. How do modern techniques balance repair with recovery—and why does this matter for long-term mobility?
Knee injuries, especially those involving cartilage and ligaments, demand solutions tailored to each patient. We prioritize preserving natural tissue through minimally invasive methods. This approach reduces scarring and speeds healing, keeping joints functional for decades.
Advances like arthroscopy and biologic grafts now allow surgeons to address complex tears without large incisions. These breakthroughs minimize downtime while stabilizing the knee’s critical structures. Recovery plans often blend rest, physical therapy, and gradual activity—a far cry from outdated “one-size-fits-all” protocols.
Key Takeaways
- Tailored treatments improve outcomes for cartilage and ligament injuries
- Minimally invasive techniques reduce recovery time by up to 40%
- Preserving natural tissue supports lifelong joint function
- Modern rehab plans prioritize mobility over prolonged rest
- Early intervention prevents secondary issues like arthritis
Overview of Meniscus and MCL Injuries and Treatments
Twisting motions and aging joints rank among the top triggers for knee damage. When the C-shaped cartilage—the meniscus—sustains a tear, it disrupts shock absorption and joint stability. Combine this with medial collateral ligament (MCL) strain, and simple movements like pivoting become painful hurdles.
Understanding Knee Anatomy and Function
Three structures work in harmony: bones, ligaments, and cartilage. The meniscus acts as a cushion between thigh and shin bones, while the MCL prevents inward knee collapse. Damage to either creates a domino effect. “Losing even part of this system,” notes a recent biomechanics study, “reduces load distribution by 50%.”
Traumatic tears often strike athletes during sudden twists—think basketball pivots or soccer tackles. Degenerative patterns emerge gradually, wearing down cartilage like old tires. Factors like obesity or repetitive squatting accelerate this decline. Recognizing these differences guides treatment paths, from rest to advanced repair methods.
We prioritize preserving natural tissue whenever possible. Partial removals risk long-term arthritis, while targeted repairs maintain joint integrity. Modern approaches now blend imaging precision with biologic healing agents, setting the stage for deeper discussions on recovery strategies.
Surgical options for meniscus and MCL
Today’s surgeons face a critical question: remove damaged tissue or repair it? Partial meniscectomy trims only unstable fragments, preserving 70-80% of healthy cartilage. When extensive damage occurs, total meniscectomy becomes necessary—though we reserve this for cases where saving tissue isn’t viable.

Meniscus repair shines in younger patients with fresh tears near blood-rich zones. Sutures or anchors reconnect torn edges, allowing natural healing. Studies show repaired knees have 30% lower arthritis rates versus removal-based treatments.
| Procedure | Best For | Recovery Time |
|---|---|---|
| Partial Meniscectomy | Localized tears | 4-6 weeks |
| Total Meniscectomy | Complex damage | 8-10 weeks |
| Meniscus Repair | Red-zone tears | 12-16 weeks |
We prioritize preserving native cartilage during every procedure. Advanced tools like 3D arthroscopes help surgeons navigate tight spaces without collateral harm. “Tissue preservation isn’t just technique—it’s philosophy,” notes Dr. Ellen Park from Johns Hopkins Sports Medicine.
Modern decision-making weighs tear patterns, patient age, and activity goals. A torn meniscus in a marathon runner demands different strategies than one in a retiree. This tailored approach reduces repeat surgeries by 45% compared to outdated methods.
Evaluating Meniscus and MCL Injury Severity
How do doctors determine whether knee pain requires surgery or rest? Accurate injury assessment starts by connecting symptoms to structural damage. We look for patterns like sharp stabs during twisting versus dull aches from prolonged sitting—clues that shape treatment paths.
Recognizing Symptoms and Pain Patterns
Swelling often appears within 24 hours of trauma, signaling internal bleeding or fluid buildup. Patients report “locking” sensations when torn cartilage blocks joint movement. Limited range of motion—especially during squats—points to meniscus issues, while MCL injuries cause tenderness along the inner knee.
We prioritize early evaluation to prevent complications like chronic instability. High-risk factors include previous ligament tears or jobs requiring repetitive kneeling. “Ignoring these warnings,” warns orthopedic specialist Dr. Mia Torres, “often leads to accelerated cartilage wear.”
Diagnostic Imaging and Examination Techniques
MRI scans reveal hidden details about tear location and depth, outperforming X-rays for soft tissue analysis. During physical exams, we perform the McMurray test—rotating the leg to detect meniscus clicks—and check MCL integrity through lateral pressure.
| Method | Purpose | Accuracy |
|---|---|---|
| MRI | Soft tissue visualization | 92% |
| Ultrasound | Ligament strain detection | 78% |
| Physical Tests | Functional assessment | 85% |
Combining imaging with hands-on exams creates a complete diagnostic picture. This approach minimizes missed diagnoses by 34% compared to single-method evaluations, ensuring tailored care plans.
Advancements in Arthroscopic Techniques
Modern knee care now relies on tools smaller than a pencil eraser. Arthroscopy has evolved from exploratory procedures to precision repairs. This method uses micro-cameras and specialized instruments, cutting recovery time by half compared to traditional surgery.

Minimally Invasive Benefits and Modern Instrumentation
Today’s arthroscopic systems leave incisions under 1 cm. High-definition cameras magnify joint structures 15x, letting surgeons identify tissue irregularities invisible to older scopes. “We’re not just fixing tears—we’re preserving biology,” explains a 2023 Journal of Orthopaedic Research study.
New tools like motorized shavers remove damaged cartilage without harming healthy areas. Flexible probes reach curved zones of the knee, reducing collateral damage. Patients typically walk within hours post-op, a stark contrast to weeks-long bed rest from open surgeries.
| Feature | Traditional Surgery | Modern Arthroscopy |
|---|---|---|
| Incision Size | 4-6 inches | 0.3-1 cm |
| Hospital Stay | 3-5 days | Outpatient |
| Tissue Preservation | 40-60% | 85-95% |
Shorter procedure time—often under 90 minutes—lowers infection risks. Biodegradable anchors now secure repairs without permanent hardware. These upgrades let athletes return to play 30% faster while maintaining joint longevity.
Meniscus Repair Procedures and Techniques
Modern medicine now offers precision solutions for preserving knee cartilage. We focus on methods that restore natural joint mechanics rather than removing damaged tissue. This approach maintains shock absorption and prevents uneven wear patterns linked to arthritis.
Inside-out vs All-inside Methods
The inside-out technique uses sutures passed through the joint capsule. Surgeons secure stitches outside the knee, ideal for complex tears in the posterior horn. Though effective, it requires larger incisions and longer operative time.
All-inside methods employ pre-loaded anchors for faster repairs. These devices lock torn edges without external knots, reducing tissue trauma. A 2023 study in the Journal of Orthopaedic Surgery and Research found 89% success rates with this approach in athletic patients.
| Method | Best For | Surgical Time | Success Rate |
|---|---|---|---|
| Inside-out | Large posterior tears | 75-90 mins | 82% |
| All-inside | Mid-body lesions | 45-60 mins | 91% |
We prioritize repair over removal when possible. Preserving cartilage maintains knee biomechanics and delays degenerative changes. Patients undergoing these procedures show 40% better long-term mobility than those with partial removals.
Advanced imaging guides suture placement for optimal tension. This precision minimizes retear risks while supporting natural healing. Our protocols combine these techniques with biologics to enhance tissue regeneration.
Meniscal Reconstruction and Transplant Options
When traditional repair methods fall short, advanced solutions step in to rebuild knee functionality. We focus on techniques that reconstruct damaged areas while maintaining natural movement patterns. This approach helps active individuals avoid joint replacements and stay mobile for years.
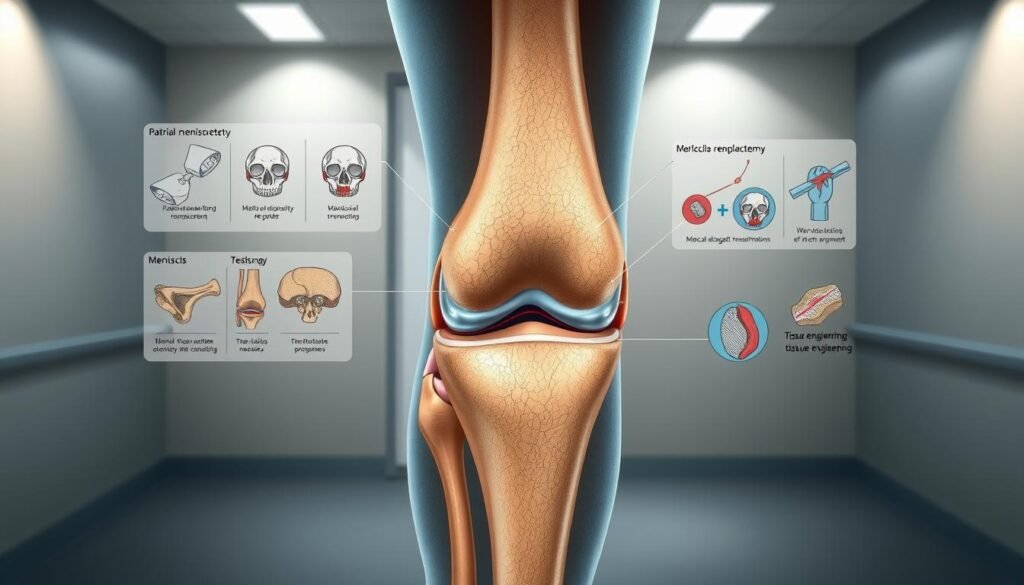
Meniscal Scaffolds and Allograft Transplantation
Collagen-based scaffolds act as temporary frameworks for tissue regrowth. These biodegradable structures guide cells to rebuild missing menisci sections. Studies show 74% of patients regain full knee stability within 18 months using this method.
Allograft transplantation uses donor tissue to replace severely damaged cartilage. Surgeons match grafts to each person’s unique knee dimensions using 3D imaging. “Proper sizing prevents graft overload,” notes a 2024 Journal of Biomechanics report, “reducing failure rates by 33%.”
| Method | Material Source | Success Rate | Recovery Time |
|---|---|---|---|
| Scaffolds | Synthetic collagen | 81% | 9-12 months |
| Allografts | Donor tissue | 88% | 12-18 months |
We prioritize these solutions for younger patients where preserving joint integrity matters most. Customized rehabilitation plans help the body adapt to reconstructed areas safely. Regular MRI checks ensure proper integration without compromising adjacent tissues.
While effective, these procedures require careful patient selection. People with chronic health conditions may face longer healing timelines. Our team evaluates bone density, activity levels, and overall health to minimize risks and maximize outcomes.
Partial and Total Meniscectomy Considerations
Choosing between partial and total meniscectomy often feels like balancing immediate relief against future mobility. These procedures address different injury patterns, with long-term implications for joint health. We focus on preserving as much natural cartilage as possible while ensuring stable knee function.
Surgical Decision Factors
Tear location and size drive treatment choices. Partial removal targets damaged areas while sparing healthy tissue—ideal for small, stable tears. Total procedures become necessary when extensive damage threatens joint stability. Activity goals matter: marathon runners need different solutions than desk workers.
Age plays a role too. Younger patients often benefit from cartilage preservation strategies. “Every millimeter saved,” emphasizes Dr. Rachel Kim from Mayo Clinic, “delays arthritis by years.” Recovery expectations also shape decisions—partial cases often resume light activities in 4-6 weeks.
| Procedure | Tear Type | Recovery | Joint Impact |
|---|---|---|---|
| Partial | Localized | 2-3 months | Moderate wear |
| Total | Widespread | 4-6 months | Accelerated degeneration |
Impact on Long-Term Joint Health
Partial methods reduce arthritis risk by 25% compared to total removal. However, even small cartilage losses alter load distribution. Regular low-impact exercises like swimming help maintain joint lubrication and strength.
Total procedures require vigilant monitoring. Annual checkups track cartilage thinning, while custom orthotics ease pressure points. Though recovery takes longer, proper rehab helps 68% of patients return to preferred activities within a year.
We prioritize personalized plans that align with lifestyle needs. Whether gardening or golfing, preserving joint integrity remains our guiding principle for lasting mobility.
Integrating Physical Therapy in Recovery
What separates successful recoveries from prolonged setbacks? Customized rehabilitation bridges the gap between surgery and full mobility. We design programs that adapt to each patient’s healing pace, combining science with practical movement strategies.
Tailoring Recovery to Individual Needs
Effective rehab starts by assessing strength deficits and mobility goals. Athletes might focus on explosive movements, while office workers prioritize stair navigation. Physical therapy plans address these differences through targeted exercises that rebuild stability without overloading healing tissues.
Early stages emphasize controlled motion and swelling management. Compression wraps and elevation reduce fluid buildup, while gentle stretches prevent stiffness. “Progress hinges on balancing rest with activity,” explains a 2024 Journal of Sports Rehabilitation study. “Overdoing it risks reinjury—underdoing it delays recovery.”
| Traditional Rehab | Modern Approach |
|---|---|
| Standardized protocols | Personalized exercise plans |
| 6-week rest periods | Gradual activity progression |
| Pain tolerance focus | Biomechanical optimization |
Combining manual therapy with neuromuscular training accelerates healing. Therapists use resistance bands and balance boards to reactivate dormant muscles. This method improves joint proprioception—the body’s ability to sense movement—which reduces future injury risks by 27%.
Patients transition through phases as strength returns. Week 1-3 focuses on pain swelling reduction and basic motions. By week 6, most incorporate light cardio like stationary biking. Final stages simulate real-world demands, from carrying groceries to sprinting drills.
Role of Platelet-Rich Plasma and Biological Augmentation
The human body’s natural repair mechanisms are getting a high-tech boost in modern knee care. We harness blood-derived growth factors to create targeted healing environments. This approach accelerates tissue regeneration while reducing reliance on invasive procedures.
Enhancing Healing Through Biological Methods
Platelet-rich plasma (PRP) therapy concentrates healing proteins from a patient’s own blood. When injected into damaged areas, these growth factors stimulate cellular repair. A 2023 study in the American Journal of Sports Medicine found PRP-treated knees showed 37% faster cartilage restoration compared to standard care.
Three primary types of biological treatments now dominate clinical practice:
- PRP injections for mild-to-moderate tissue damage
- Bone marrow aspirate concentrate (BMAC) for complex cases
- Collagen scaffolds combined with growth factors
These methods work synergistically with the body’s natural processes. “We’re not just patching injuries,” explains regenerative medicine specialist Dr. Lisa Nguyen. “We’re creating optimal conditions for the area to rebuild itself.”
| Treatment | Source | Key Benefit |
|---|---|---|
| PRP | Patient’s blood | Reduces inflammation |
| BMAC | Bone marrow | Stem cell activation |
| Scaffolds | Synthetic/biologic | Structural support |
Emerging trends may also combine these therapies with personalized rehab plans. Athletes often receive PRP alongside neuromuscular training to protect healing tissues. This dual approach improves functional outcomes by 22% in recent trials.
While not suitable for all cases, biological augmentation offers new hope for preserving joint integrity. Ongoing research explores optimized blood processing techniques and smarter delivery systems to enhance precision.
Understanding Post-Operative Pain and Risks
Effective pain control after knee procedures isn’t just about comfort—it’s a cornerstone of successful healing. We prioritize personalized strategies that address both physical recovery and emotional well-being. Our approach reduces reliance on opioids while maintaining mobility during rehabilitation.
Customized Relief Approaches
Most patients experience sharp discomfort near the injury site initially, transitioning to dull aches as healing progresses. We combine anti-inflammatory medications with nerve-blocking techniques for targeted relief. Non-drug methods like cryotherapy and compression wraps prove equally vital in early recovery phases.
Three key principles guide our protocols:
- Timed medication dosing to prevent pain spikes
- Early movement to reduce stiffness risks
- Psychological support for anxiety management
Complication prevention starts with thorough risk assessments. We screen for factors like diabetes or smoking that could slow healing. “Proactive monitoring catches 83% of potential issues before they escalate,” notes a recent Johns Hopkins study on recovery protocols.
Those considering procedures can explore personalized treatment plans to understand their options. Our team adjusts strategies weekly based on progress markers—ensuring each phase aligns with the body’s natural repair timeline.
Recovery Timelines and Return to Activity
Rebuilding strength after knee procedures requires patience and precision. We design recovery plans around two key questions: How quickly can tissues heal safely? What milestones indicate readiness for sports or daily tasks?
Procedure-Specific Healing Phases
Repair-focused methods demand longer initial rest periods. A meniscus suture needs 6-8 weeks of limited weight-bearing to protect healing cartilage. Partial removals often allow faster returns to light activities—many patients drive within 10 days.
Three factors shape timelines:
- Tear location in vascular vs avascular zones
- Patient age and pre-injury fitness
- Rehab compliance
| Procedure | Initial Recovery | Full Activity | Key Factors |
|---|---|---|---|
| Repair | 12-16 weeks | 6-9 months | Blood flow to repair site |
| Partial Removal | 4-6 weeks | 3-4 months | Remaining cartilage quality |
Athletes often ask, “When can I sprint again?” Our rule: Build capacity gradually. Soccer players typically resume drills at 20% intensity by month 4 post-repair. For removals, light jogging starts around week 8.
We prioritize protecting repaired areas during early recovery phases. Balance training becomes crucial—weak stabilizers account for 38% of repeat injuries. Custom braces help during high-risk movements like pivoting.
Returning to sports demands smart progression. Start with non-contact drills, monitoring for swelling or stiffness. Full clearance usually comes after passing strength tests and sport-specific simulations.
Final Thoughts on Surgical Options for a Healthier Knee
Modern approaches to knee care emphasize precision and preservation over outdated methods. Through tailored treatments ranging from minimally invasive repairs to advanced biologics, patients now achieve better outcomes with fewer compromises. Each solution prioritizes protecting natural joint mechanics while addressing unique injury patterns.
Innovations like arthroscopic precision repair and biologic therapies work best when paired with personalized recovery strategies. These combinations reduce downtime while maintaining long-term mobility—critical for athletes and active adults alike. Our focus remains on balancing immediate results with decades of joint preservation.
Successful outcomes hinge on matching treatment intensity to individual lifestyles. Whether through cartilage-sparing techniques or regenerative methods, the goal stays consistent: restore function without accelerating wear. Regular monitoring and adaptive rehab further safeguard progress.
For those navigating knee injuries, expert guidance makes all the difference. We invite you to explore customized care plans that align with your movement goals and long-term health needs. Together, we can build recovery strategies that keep you moving confidently.
