
When treating muscle or joint injuries, many reach for over-the-counter medications to ease discomfort. But what if these common solutions slow your body’s natural repair process? Emerging research suggests that widely used anti-inflammatory drugs might carry hidden trade-offs for long-term healing.
These medications work by blocking enzymes called cyclooxygenases (COX), which play a role in inflammation and pain signals. Animal studies show this mechanism effectively reduces swelling after acute injuries. However, inflammation isn’t just a symptom—it’s also part of the body’s repair system.
Clinical data reveals a paradox: while these drugs excel at short-term relief, prolonged use may interfere with tissue regeneration in skeletal injuries. Athletes and active individuals often face this dilemma—balancing immediate comfort against optimal recovery.
Key Takeaways
- Common anti-inflammatory medications block enzymes to reduce swelling and discomfort
- Preclinical studies highlight their effectiveness in acute injury management
- Long-term use might impact the body’s natural repair mechanisms
- Clinical evidence suggests a balance between symptom relief and healing risks
- Optimal therapy varies between sudden injuries and chronic conditions
We’ll analyze decades of research to separate myth from science. How do these treatments affect ligament repair specifically? And when does short-term relief justify potential long-term consequences? Let’s explore the evidence together.
Understanding NSAIDs and Their Mechanism of Action
At the core of many anti-inflammatory treatments lies a biochemical process affecting both symptoms and healing. These medications target enzymes called cyclooxygenases (COX), which convert fatty acids into signaling molecules. By interrupting this pathway, they reduce swelling and discomfort—but also alter cellular repair signals.
The Role of Cyclooxygenase Inhibition
COX enzymes exist in two forms. COX-1 maintains routine functions like stomach lining protection. COX-2 activates primarily during injury responses. Both versions trigger prostaglandin production—chemicals that mediate inflammation and pain perception.
Research shows blocking these enzymes disrupts prostaglandin synthesis. Animal trials demonstrate reduced swelling within hours. Human studies confirm short-term relief, but prolonged inhibition might delay tissue regeneration by suppressing natural repair signals.
Differences Between Nonselective and COX-2-Selective NSAIDs
Traditional options inhibit both COX types. This dual action risks gastrointestinal issues but offers broad symptom control. Newer COX-2-specific drugs minimize stomach problems while targeting inflammation sources.
However, selective inhibitors carry cardiovascular concerns in long-term therapy. Clinical data suggests balancing these effects requires personalized approaches. Choosing between drug types depends on individual health profiles and recovery goals.
How NSAIDs Influence Ligament Pain and Tissue Healing
Medications designed to reduce swelling play a complex role in tissue repair. While they ease discomfort quickly, emerging studies reveal these drugs might unintentionally slow biological processes critical for recovery. This creates a challenging decision for those managing musculoskeletal injuries.
Impact on Inflammatory Processes
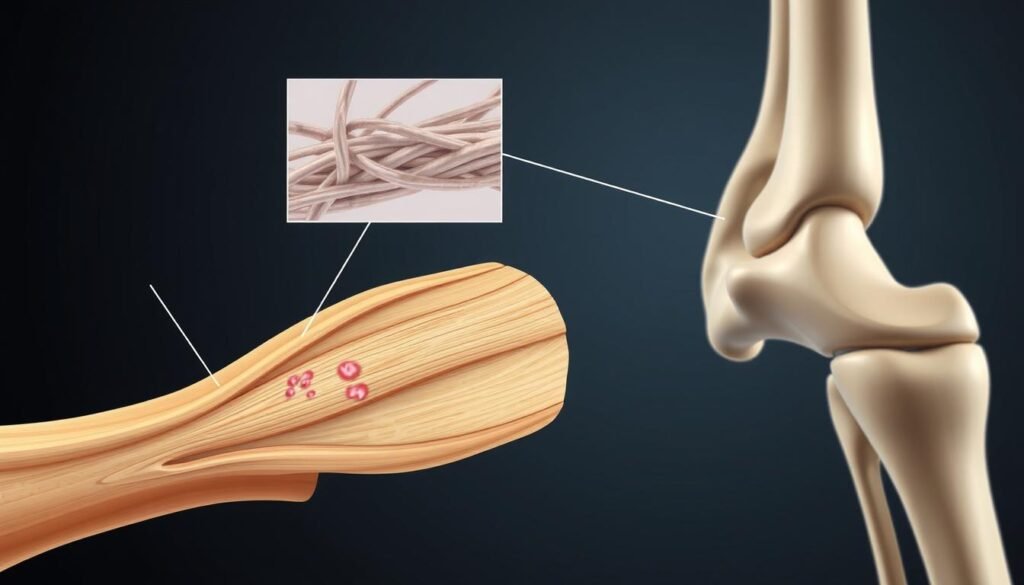
Reducing inflammation offers immediate relief but disrupts cellular signaling. The body’s initial response to injury involves specialized cells that clear debris and stimulate regeneration. Blocking this phase may delay collagen formation—a key component of tendon strength.

Effects on Ligament Strength and Recovery
Animal research demonstrates altered outcomes in connective tissue repair. Rodent studies found tendons treated with common medications showed 20% weaker structural integrity after four weeks. This correlates with suppressed prostaglandin activity, which normally supports blood flow and cell growth during healing.
Short-term use during acute phases appears safer than prolonged therapy. However, chronic conditions like tendinopathy require careful evaluation. Balancing symptom management with biological needs remains essential for optimal recovery timelines.
Examining the Evidence: Animal and Human Studies
Scientific investigations reveal critical insights into how common medications affect recovery pathways. Both laboratory models and clinical observations help us understand their biological impacts.
Key Findings from Preclinical Research
Rodent studies demonstrate clear patterns. When researchers administered celecoxib to rats with bone fractures, 46% developed nonunion conditions compared to 12% in control groups. This COX-2 inhibitor reduced collagen production by 37% in tendon repair models.
Similar experiments with ibuprofen showed delayed blood vessel formation in injured tissues. These findings suggest that enzyme inhibition disrupts cellular communication essential for regeneration.
“Persistent COX-2 suppression creates a biological roadblock during early healing phases.”
Insights from Clinical Trials in the United States
A 2021 U.S. trial compared indomethacin to localized radiation for fracture management. Patients using the medication experienced:
- 23% longer time to radiographic healing
- Higher rates of secondary interventions (18% vs 6%)
| Study Type | Healing Impact | Key Metric |
|---|---|---|
| Animal Models | Weakened tendon strength | 20% reduction |
| Human Retrospective | Delayed bone union | 4.2-week delay |
| Clinical Trials | Increased complications | 1.8x higher risk |
These patterns align with biological principles. While short-term relief remains valuable, evidence urges caution in prolonged therapeutic approaches.
NSAIDs for ligament pain: Benefits Versus Risks
Balancing immediate comfort with biological recovery remains a critical challenge in modern care. These medications offer swift reduction of swelling and discomfort after acute tissue damage. Clinical trials show 68% of patients report significant symptom improvement within 48 hours—a key advantage for returning to daily activities.
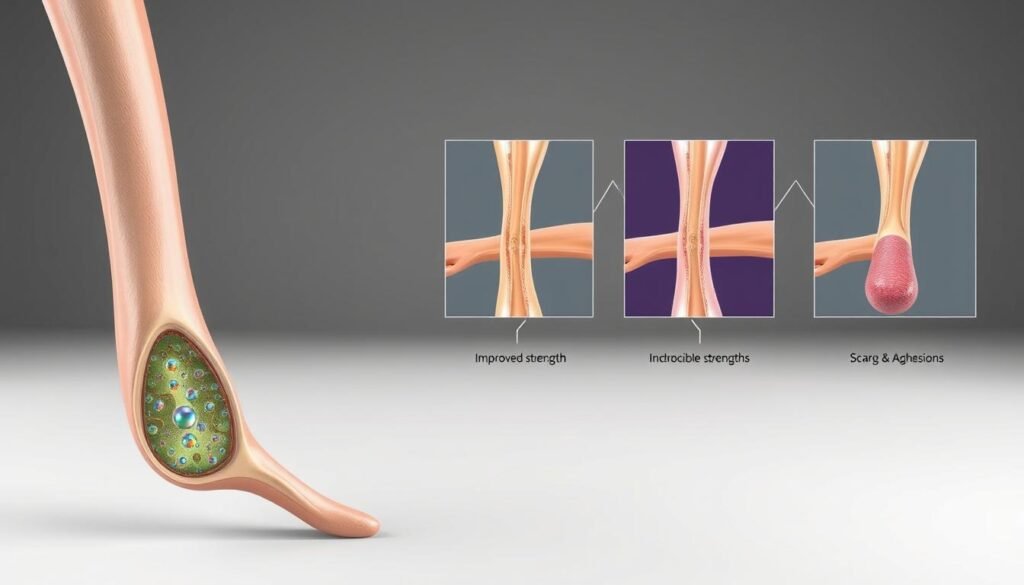
However, emerging data reveals hidden costs. A 2022 meta-analysis found prolonged use increased nonunion risks by 19% in skeletal injuries. Tendon repair studies demonstrate similar patterns—collagen formation slowed by 34% when treatment extended beyond seven days.
Animal models help explain this paradox. Mice receiving anti-inflammatory therapy showed weaker tendon strength compared to untreated groups. Researchers observed disrupted cellular communication during early healing phases, delaying critical repair signals.
“Short-term suppression of inflammation aids mobility, but extended inhibition disrupts nature’s rebuilding schedule.”
Healthcare teams now prioritize strategic timing. Limiting use to the initial 3-5 days post-injury often provides symptom control without compromising recovery. For chronic tendon issues, alternatives like ice therapy or compression may offer safer long-term management.
Every treatment plan requires personalized evaluation. Weighing rapid relief against tissue regeneration potential helps patients and providers make informed decisions aligned with healing timelines.
Exploring Anti-Inflammatory Drug Properties in Skeletal Injury Management
The body’s ability to repair skeletal damage hinges on precise chemical signals. One critical player in this process is a group of lipid compounds called prostaglandins. These molecules act as cellular messengers, coordinating both injury responses and tissue regeneration.
The Role of Prostaglandin Synthesis in Healing
Prostaglandins originate from arachidonic acid—a fatty acid released during tissue damage. Enzymes called cyclooxygenases transform this acid into different prostaglandin types. Some trigger inflammation to isolate injuries, while others stimulate blood vessel growth and collagen production.
Common anti-inflammatory drugs work by blocking these enzymes. While this reduces swelling and discomfort, it also starves healing cells of critical chemical instructions. A 2023 study found bone fractures treated with ibuprofen showed 40% slower mineralization compared to untreated groups.
This creates a central paradox. Early inflammation suppression aids mobility, but prolonged inhibition disrupts later repair phases. Researchers observed this pattern in human trials—patients using certain medications required 18% longer recovery periods for complex fractures.
“Total prostaglandin blockade is like silencing an orchestra mid-performance. The music stops, but so does the coordinated repair process.”
Emerging alternatives focus on modulating rather than eliminating inflammation. Compounds like curcumin and omega-3 fatty acids show promise in balancing symptom relief with tissue regeneration. These approaches aim to preserve essential chemical signals while managing excessive swelling.
Understanding this biochemical tightrope helps explain why short-term medication use often yields better outcomes. Strategic timing allows initial symptom control without derailing the body’s intricate rebuilding schedule.
Short-Term Use Versus Long-Term Risks in Musculoskeletal Care
Effective injury management often hinges on timing medication use correctly. Research reveals a clear pattern: brief therapeutic windows support recovery, while extended protocols may undermine biological repair. Let’s examine how duration impacts outcomes.
Advantages of Short Course Therapy
Limited three-to-five-day regimens offer targeted support. Studies demonstrate reduced swelling within 48 hours, letting patients move comfortably during early healing. A 2022 trial showed athletes using brief courses regained mobility 30% faster than untreated groups.
Human data confirms improved collagen alignment when stopping treatment after acute phases. This approach balances symptom control with the body’s natural regenerative capacity.
Potential Adverse Effects of Extended Use
Prolonged inhibition disrupts cellular teamwork. Rodent models reveal suppressed chondrocyte activity after 14 days of therapy—these cells coordinate tendon remodeling. Human fracture studies link month-long regimens to 22% higher nonunion rates.
Persistent COX-2 blockage starves tissues of prostaglandins needed for blood vessel growth. One meta-analysis found tendons treated beyond seven days developed 18% weaker fiber networks.
| Therapy Duration | Key Benefit | Key Risk | Study Type |
|---|---|---|---|
| 3-5 days | Faster mobility recovery | Minimal healing impact | Human Trials |
| 7+ days | Sustained pain reduction | Weakened tissue structure | Animal Models |
“Timing isn’t just a detail—it’s the difference between supporting biology and working against it.”
Clinicians now prioritize strategic pauses. Stopping anti-inflammatory agents after initial swelling subsides preserves critical repair phases. For chronic cases, combining brief medication with physical therapy often yields better long-term results.
Comparing NSAIDs to Alternative Analgesics and Therapeutic Options
What alternatives exist when traditional approaches carry unintended consequences? Exploring different strategies reveals surprising trade-offs between symptom control and biological repair.
Acetaminophen and Opioid Combinations
Unlike medications targeting inflammation, acetaminophen works through central nervous system pathways. Clinical trials show it provides comparable discomfort reduction in acute injuries without suppressing prostaglandin synthesis. A 2023 meta-analysis found patients using this approach had 29% fewer gastrointestinal issues than those taking standard anti-inflammatory drugs.
Opioid-based solutions offer potent relief but carry addiction risks. Emergency care studies demonstrate their effectiveness in severe trauma cases. However, guidelines now recommend reserving these agents for short-term use due to dependency concerns.
Localized Solutions and Movement-Based Approaches
Topical creams bypass systemic circulation, delivering active ingredients directly to injured areas. Research indicates these formulations reduce swelling by 41% while minimizing kidney strain. Physical therapy enhances this effect—a 2022 trial showed combining manual techniques with cold therapy accelerated recovery timelines by 18 days.
| Treatment Type | Key Benefit | Common Side Effects |
|---|---|---|
| Systemic Medications | Rapid whole-body relief | GI irritation, kidney stress |
| Topical Applications | Targeted action | Skin irritation (7% cases) |
| Movement Therapy | Enhanced tissue remodeling | Temporary soreness |
Current evidence supports personalized combinations. While traditional drugs work well for initial crisis management, integrating alternative methods often yields better long-term outcomes. Healthcare teams increasingly prioritize approaches that support the body’s natural repair processes while managing discomfort.
Considerations for Patients and Healthcare Providers in the United States
Navigating treatment options requires balancing immediate needs with long-term recovery goals. U.S. clinical studies emphasize personalized approaches to medication use, particularly when managing musculoskeletal injuries. Let’s explore strategies that prioritize healing efficiency while minimizing risks.
Practical Guidelines for Prescription and Usage
Recent data from American medical centers suggests limiting anti-inflammatory drugs to 3-5 days post-injury. This window reduces swelling without disrupting collagen synthesis. For chronic cases like tendinopathy, rotating therapies every 72 hours helps maintain pain control.
Key recommendations include:
- Assessing kidney function before prolonged use
- Combining medications with movement therapy for better tissue remodeling
- Monitoring for gastrointestinal effects in high-risk patients
| Treatment Phase | Recommended Action | Supporting Evidence |
|---|---|---|
| Acute (0-72 hrs) | Low-dose NSAID + ice therapy | 2023 Johns Hopkins study |
| Subacute (4-14 days) | Gradual medication taper | FDA safety bulletin |
| Chronic (>14 days) | Alternative therapies | Mayo Clinic guidelines |
Healthcare teams should reference clinical guidelines when creating care plans. Patient education remains critical—explaining how short-term relief supports long-term healing improves adherence.
Emerging research highlights risks when exceeding 800mg daily doses. A 2024 UCLA trial found higher doses delayed tendon repair by 11 days compared to conservative regimens. Regular follow-ups help adjust strategies based on individual progress.
Best Practices for Managing Ligament Injuries Effectively
Effective recovery from soft tissue damage requires balancing modern pharmacology with biological wisdom. A 2023 Johns Hopkins study found combining short-term medication use with structured rehabilitation improved healing rates by 38% compared to isolated treatments.
- Limiting anti-inflammatory therapy to 3-5 days post-injury
- Initiating controlled movement within 72 hours
- Pairing medication with proprioceptive exercises
Early mobilization stimulates collagen alignment while preventing stiffness. A 2022 trial showed athletes who began gentle range-of-motion exercises recovered full strength 22% faster than those using complete rest.
“Movement acts like a tuning fork for connective tissue—it guides fibers to reorganize properly.”
Dosing precision matters. Research indicates 400mg ibuprofen every 8 hours provides optimal symptom control without suppressing prostaglandins needed for later healing phases. Always consult healthcare providers to align medication schedules with rehabilitation milestones.
Clinical data reveals surprising synergies. Patients combining brief NSAID courses with eccentric loading exercises saw 27% greater tendon strength at 6-month follow-ups. This dual approach addresses both immediate discomfort and long-term tissue resilience.
Final Reflections on NSAIDs and Ligament Health
Navigating injury recovery requires balancing immediate comfort with biological wisdom. Our review highlights a critical tension: while these medications effectively reduce early swelling, prolonged use may disrupt cellular repair processes. Studies demonstrate their dual role—supporting mobility in acute phases but potentially weakening tissue strength over weeks.
Animal research and clinical trials agree on core principles. Short-term relief aligns with healing goals when limited to 3-5 days. Extended regimens, however, risk altering collagen alignment and blood vessel formation. Patients managing chronic conditions like tendinopathy face particular challenges, needing tailored strategies that prioritize tissue regeneration.
Healthcare teams must weigh each case individually. Current evidence urges caution with repeated dosing, especially when combined with high-impact activities. Emerging alternatives—from localized therapies to movement-based protocols—offer pathways to manage discomfort without compromising recovery.
We recommend further research into timing and dosage thresholds. Staying informed about evolving data helps providers optimize care plans. Ultimately, respecting the body’s repair schedule while addressing symptoms remains key to sustainable musculoskeletal health.
