
What if the ache in your knee isn’t just a minor strain? Many active individuals dismiss discomfort as temporary, but ignoring certain signs could lead to bigger problems. The medial collateral ligament (MCL) is a critical stabilizer for your joint, and damage here often reveals itself through specific patterns.
We’ve seen countless cases where early recognition of these patterns makes a difference. A sudden twist or impact can strain the inner part of your knee, triggering sensations ranging from stiffness to sharp twinges. Without proper care, even mild issues might escalate into instability during routine movements.
But how do you distinguish between general soreness and something more serious? The answer lies in understanding how the MCL functions. This band of tissue connects your thighbone to your shinbone, absorbing stress during activities like pivoting or jumping. When compromised, it sends clear signals—swelling, tenderness, or difficulty bearing weight.
Key Takeaways
- The MCL stabilizes the inner knee and is prone to injury during sudden movements.
- Early signs include localized tenderness and stiffness after activity.
- Severity ranges from mild discomfort to difficulty walking or standing.
- Ignoring symptoms may lead to chronic instability or secondary injuries.
- Consult a healthcare provider for persistent or worsening issues.
Exploring MCL Pain Symptoms
Not all knee discomfort fades with rest; some patterns hint at deeper issues. A sudden twist or impact often triggers immediate sensations—like a distinct “pop” sound—followed by sharp inner knee discomfort. This audible cue frequently accompanies difficulty standing or shifting weight evenly.

| Severity Level | Key Signs | Mobility Impact |
|---|---|---|
| Mild | Localized tenderness | Minimal walking changes |
| Moderate | Visible swelling | Partial weight-bearing |
| Severe | Bruising + instability | Walking assistance needed |
Inner knee sensitivity typically appears first. Light pressure along the medial joint line often reveals specific sore spots. Within hours, inflammation may spread, creating visible puffiness or purple discoloration.
Many patients describe a “wobbly” feeling when attempting stairs or pivots. This instability stems from the medial collateral ligament’s role in stabilizing sideways motions. Early recognition helps prevent compensatory movements that strain other joint structures.
Understanding the Medial Collateral Ligament (MCL) in Our Knee
Knee stability relies on a complex network of tissues working in harmony. Among these, the medial collateral ligament stands out as a primary defender against inward knee collapse. This thick band connects the thighbone (femur) to the shinbone (tibia), forming a critical barrier during lateral movements.
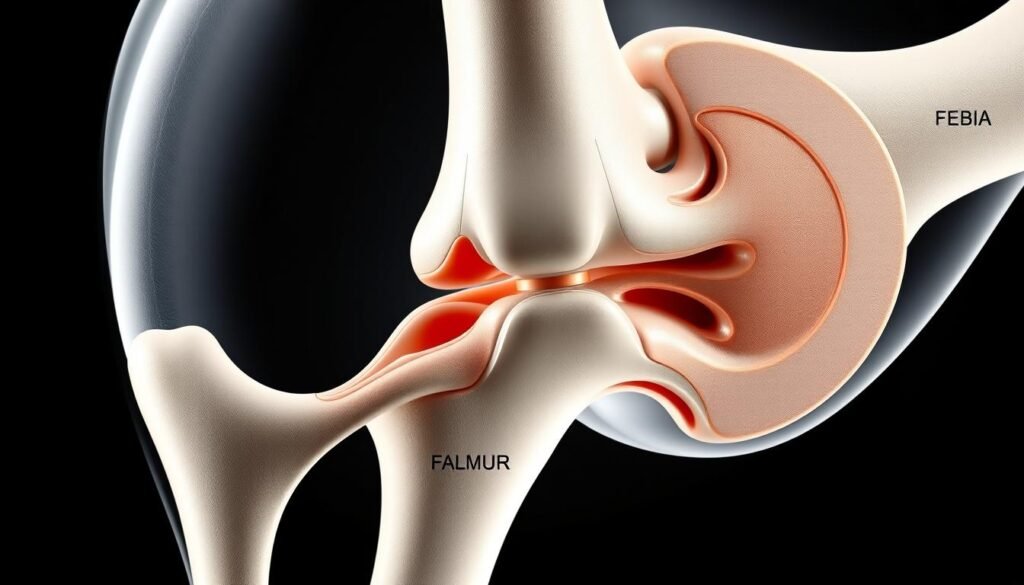
Anatomy and Function of the MCL
The medial collateral ligament’s structure reveals why it’s so vital. Originating from the femur’s medial epicondyle, it spans downward to attach firmly on the tibia. Unlike thinner ligaments, its dense fibers can withstand significant stress.
“This design allows it to act like a seatbelt for your knee,” notes a sports medicine specialist. Its robust build helps maintain alignment during twists or impacts that could otherwise destabilize the joint.
How the MCL Contributes to Knee Stability
Every step or pivot tests the ligament’s ability to maintain alignment. It primarily resists valgus forces—those pushing the knee inward. When functioning properly, it works with adjacent tendons to distribute impact evenly.
Damage here compromises the entire joint’s balance, emphasizing its role as a stabilizer. Proper care ensures this fibrous bridge between femur and tibia continues supporting daily movements seamlessly.
Causes and Mechanisms Behind MCL Injuries
A single misstep can compromise the knee’s crucial stabilizers. We often see damage occur when force strikes the outer knee during contact sports, pushing the joint inward. This lateral impact stretches or tears the medial collateral ligament instantly.
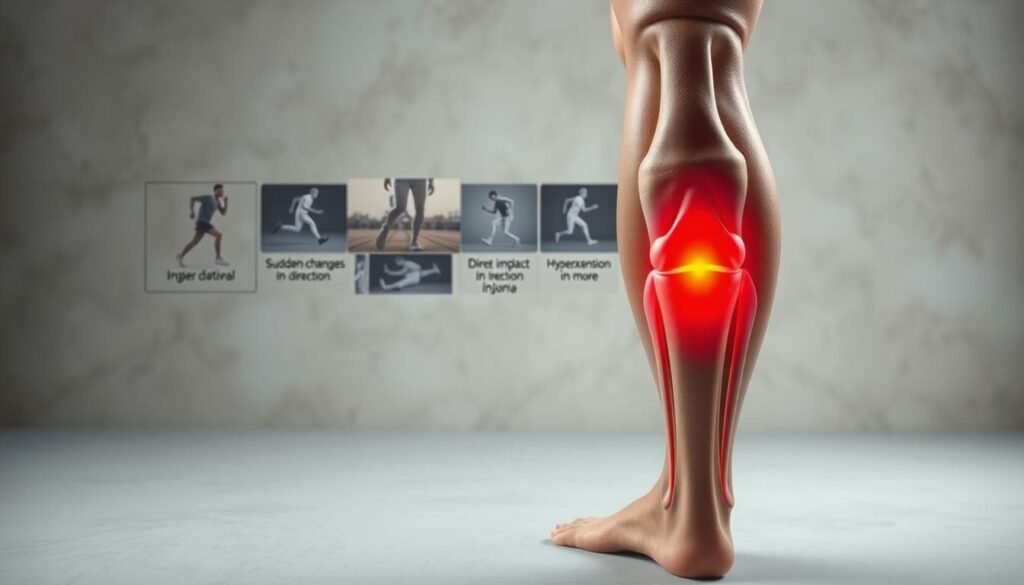
Football players and skiers face particularly high risks. Tackles or collisions in football create perfect conditions for these knee injuries. Similarly, ski bindings that don’t release properly during falls often lead to twisting forces that overstress the ligament.
“The majority of complete tears we treat come from high-impact sports where players can’t control their momentum,” notes a collegiate sports therapist.
| Cause | Mechanism | Common Sports |
|---|---|---|
| Direct contact | Outside knee impact | Football, rugby |
| Twisting motion | Sudden direction change | Basketball, skiing |
| Improper landing | Hyperextension | Gymnastics, volleyball |
Non-contact actions like pivoting sharply or landing awkwardly also rank high. These movements strain the ligament’s capacity to stabilize sideways motion. Weightlifters sometimes experience gradual damage from repetitive deep squats.
Understanding these patterns helps athletes modify techniques. Proper conditioning and protective gear reduce risks significantly. Early intervention prevents minor sprains from becoming chronic stability issues.
Differentiating MCL Sprains, Tears, and Other Knee Injuries
Knee injuries often involve multiple structures working together. When force pushes the joint inward or twists a planted foot, the medial collateral ligament may stretch beyond its limits. This results in either a partial tear (sprain) or complete rupture.
Sprains Versus Complete Ruptures
A sprain indicates stretched fibers with partial tearing. Patients typically maintain some stability. Complete tears, however, create noticeable looseness. We categorize these injuries into three grades:
- Grade 1: Mild stretching with minimal fiber damage
- Grade 2: Partial tear causing moderate instability
- Grade 3: Full rupture requiring extended recovery
Common Injury Combinations
Nearly half of all knee trauma involves this ligament. High-impact accidents frequently damage adjacent structures:
| Associated Injury | Mechanism | Detection Method |
|---|---|---|
| Anterior cruciate ligament tear | Sudden stops/pivots | Lachman test + MRI |
| Meniscus damage | Twisting under load | Joint line tenderness exam |
“Combined injuries complicate treatment plans. Imaging helps us spot hidden damage that physical exams might miss.”
Proper diagnosis guides rehabilitation strategies. Isolated grade 1-2 injuries often heal with rest, while complex cases may need surgical evaluation. Early assessment prevents long-term joint issues.
Recognizing the Warning Signs and Symptoms
Certain sensations in your joint demand immediate attention. A sudden “pop” during activity often signals trouble, followed by sharp discomfort along the inner side. This distinct sound frequently pairs with visible changes within hours.
We regularly see swelling emerge as one of the first physical indicators. The medial area may appear puffy, sometimes spreading toward the thigh or calf. Light pressure along this region typically triggers noticeable tenderness, making even gentle touches uncomfortable.
Discoloration often develops over 1-2 days, ranging from faint redness to pronounced bruising. “The ‘black and blue’ pattern helps us gauge injury severity,” explains a sports medicine physician. Mobility challenges like instability when shifting weight or climbing stairs also raise red flags.
| Symptom | Timeline | Action Needed |
|---|---|---|
| Audible pop | Immediate | Stop activity |
| Localized swelling | 0-6 hours | Apply ice |
| Bruising | 24-48 hours | Seek evaluation |
Catching or locking sensations suggest possible involvement of other structures. These mechanical issues often worsen without proper care. Early intervention helps prevent compensatory movements that strain unaffected areas.
Non-Surgical Treatment Options for MCL Pain
Effective recovery begins with proven conservative approaches. Most ligament injuries heal successfully without surgery due to strong natural blood flow to the area. Our team prioritizes methods that support the body’s healing process while maintaining mobility.
RICE Method and Pain Relievers
We start every treatment plan with the RICE protocol:
- Rest: Avoid activities stressing the joint for 1-2 weeks
- Ice: Apply cold packs 4x daily to reduce swelling
- Compression: Elastic wraps provide gentle support
- Elevation: Keep the leg raised above heart level when resting
Over-the-counter NSAIDs like ibuprofen help manage discomfort during the first 72 hours. We adjust dosages based on individual needs and monitor progress closely.
Role of Crutches and Knee Bracing in Early Recovery
Protective gear plays a vital role in healing. Hinged braces limit sideways motion while allowing natural bending. Patients typically wear them 3-6 weeks depending on tear severity.
Crutches help distribute weight evenly during walking. We recommend partial weight-bearing for 7-10 days before gradually increasing activity. Most people transition to full mobility within 2 weeks for mild cases.
“Proper bracing and load management accelerate recovery by 40% compared to unprotected healing,” notes a physical therapy researcher.
How Physical Therapy Helps Restore Knee Function
Regaining full knee mobility requires more than just time—it demands strategic movement. We design rehabilitation programs that rebuild strength while protecting healing tissues. Early-phase exercises focus on gentle motions to prevent stiffness, progressing to resistance training as stability improves.
Our three-phase approach includes:
- Phase 1: Range-of-motion drills like heel slides and seated leg extensions
- Phase 2: Quadriceps strengthening with mini-squats and step-ups
- Phase 3: Sport-specific agility work for athletes
Cycling proves particularly effective for maintaining joint mobility without impact. A recent study showed patients using stationary bikes regained 30% more flexibility than those relying solely on rest. “Controlled movement stimulates blood flow, which accelerates healing,” explains a certified orthopedic specialist.
For contact sports like soccer or basketball, we simulate game scenarios using lateral shuffle drills and pivoting exercises. This tailored preparation helps athletes return to play with confidence while reducing re-injury risks. Consistent participation typically yields noticeable improvements within 4-6 weeks.
“The right combination of strength training and functional movements makes all the difference in long-term recovery outcomes.”
When to Use Support Devices Like Knee Braces and Crutches
Support tools can make or break your recovery timeline after a knee injury. We recommend hinged braces during early healing phases to block sideways motion while allowing natural bending. These devices typically stay on for 3-7 days post-injury, depending on severity.
Crutches help maintain mobility without overloading healing tissues. Most patients use them 2-5 days before transitioning to partial weight-bearing. Our team emphasizes temporary use – prolonged reliance can delay muscle reactivation.
Key principles guide our approach:
- Lightweight materials prevent joint stiffness
- Daily brace checks ensure proper fit
- Gradual weaning preserves natural stability
Time spent in braces rarely exceeds two weeks for isolated injuries. We combine support devices with early motion exercises to prevent atrophy. Follow-up assessments determine when to phase out aids completely.
Proper use accelerates recovery while avoiding dependency. Always consult your specialist before adjusting brace settings or ditching crutches early. Temporary support today prevents long-term instability tomorrow.
