
What if the lingering discomfort in your leg isn’t just “normal soreness” but a sign of deeper structural imbalance? Many dismiss recurring weakness during routine movements, unaware that ligament damage or mechanical misalignment could silently sabotage their mobility.
When the connection between bones like the femur and patella weakens, simple tasks—like climbing stairs or standing up—become unpredictable challenges. This isn’t just about temporary pain. It’s about how torn tissues or cartilage wear reshape your body’s ability to function safely.
Overuse, sudden twists, or untreated trauma often trigger these issues. Left unaddressed, they can spiral into chronic limitations. That’s why recognizing early signs—like a shaky sensation or clicking sounds—is critical for reclaiming control.
Key Takeaways
- Persistent wobbling during movement often signals ligament or patellar damage.
- Daily activities like walking or sitting may worsen untreated joint weaknesses.
- Common causes include repetitive strain, acute injuries, or cartilage deterioration.
- Early symptom identification prevents long-term mobility loss.
- Personalized treatment plans combine strengthening exercises and clinical therapies.
Our guide cuts through the confusion, offering science-backed strategies to stabilize your stride. From targeted exercises to advanced recovery methods, we’ll help you rebuild confidence in every step.
Understanding the Knee Joint and Its Role in Stability
Mobility hinges on the seamless interaction of bones, ligaments, and cartilage within one of the body’s most complex joints. Three primary bones—the femur (thigh bone), tibia (shin bone), and patella (kneecap)—form its foundation. These structures work together to absorb impact while enabling fluid motion.
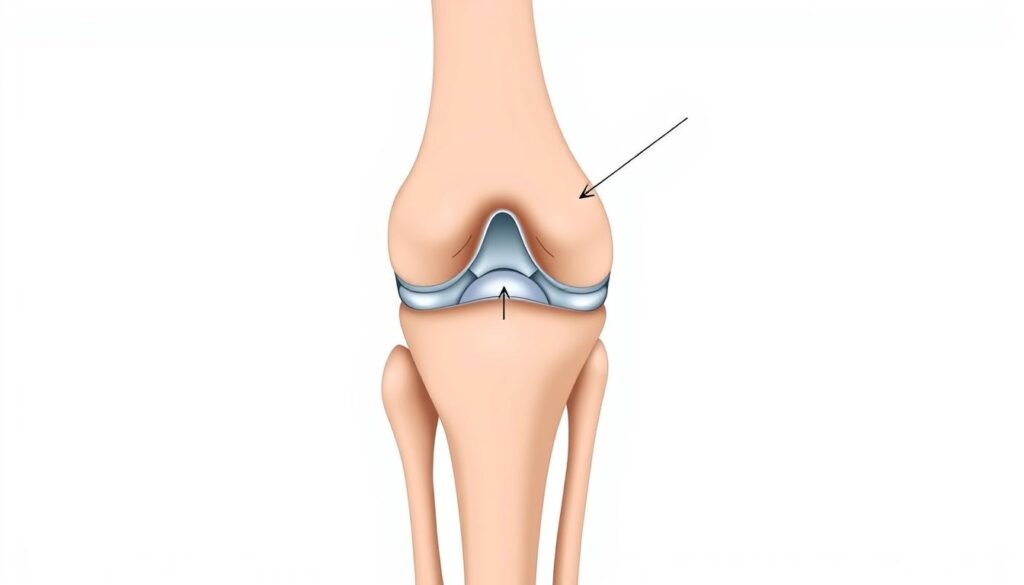
Four key ligaments act as biological cables, connecting the femur to the tibia. The ACL and PCL control forward-backward movement, while the MCL and LCL prevent sideways shifting. Rounded femoral condyles and crescent-shaped menisci further stabilize the joint, distributing weight evenly during activities like walking or squatting.
Proper alignment of these components is critical. When bones and soft tissues maintain their natural positions, stress spreads uniformly. Misalignment, however, strains specific areas, accelerating wear or causing instability.
Understanding this anatomy helps professionals pinpoint issues during diagnosis. For example, lax ligaments or damaged menisci alter how forces travel through the joint. This knowledge guides targeted assessments, which we’ll explore in later sections.
Recognizing Signs and Symptoms of Knee Instability
Have you ever felt your joint suddenly give way during a simple movement? This unpredictable buckling often signals deeper issues within the complex network of tissues supporting your stride. Early detection of these red flags can prevent minor discomfort from evolving into chronic limitations.

Common Symptoms: Pain, Swelling, and Locking
Persistent pain during routine tasks like climbing stairs often serves as the first warning. Swelling around the joint may follow, creating stiffness that limits movement. Some report a clicking sensation or temporary “locking” when attempting to straighten their leg fully.
Abnormal sensations—like the leg twisting awkwardly or feeling unstable—frequently point to ligament damage. These episodes might occur sporadically, making them easy to dismiss. However, recurring instability during daily activities demands attention before wear escalates.
Indicators Requiring Professional Evaluation
A loud “pop” accompanied by immediate swelling suggests acute trauma needing urgent care. Difficulty bearing weight or persistent warmth around the area also warrants assessment. Professionals use advanced imaging to identify tears or cartilage deterioration invisible to the naked eye.
Mild cases often improve with rest and targeted exercises. Severe or worsening symptoms, however, require structured treatment plans. Combining at-home care with clinical therapies offers the best path to restoring confident mobility.
Managing Knee instability after injury: A Comprehensive Approach
Rebuilding strength post-trauma requires a layered strategy that balances rest with gradual activity. Immediate care often begins with the RICE protocol—rest, ice, compression, and elevation—to reduce swelling and protect damaged tissues. This foundational step creates the optimal environment for healing.

Once acute symptoms subside, structured physical therapy becomes essential. Therapists design programs targeting quadriceps and hamstrings—muscles critical for joint support. Low-impact exercises like leg lifts or resistance band work rebuild strength without overloading vulnerable structures.
Three pillars define successful recovery:
- Early mobilization: Gentle movements prevent stiffness while promoting blood flow
- Progressive loading: Gradually increasing activity levels avoids re-injury
- Personalization: Plans adapt to injury severity and lifestyle demands
Specialists use diagnostic imaging and functional tests to identify specific weaknesses. This data-driven approach ensures therapy addresses root causes rather than just symptoms. For example, balance drills might correct proprioception issues contributing to instability.
Consistency matters most. Patients combining clinic visits with home routines typically regain stability faster than those relying solely on passive treatment. Regular progress checks allow timely adjustments, keeping recovery on track.
Identifying Injury-Related Causes and Ligament Damage
Every sudden twist or awkward landing could be the unseen culprit behind a compromised joint. Structural weaknesses often stem from two primary sources: acute trauma and repetitive strain. Both scenarios disrupt the delicate balance required for smooth movement.
Impact of Traumatic Injuries and Overuse
High-impact sports like basketball or soccer frequently lead to abrupt ligament tears. A forceful pivot or collision can overstretch connective tissues beyond their limits. Partial tears reduce stability, while complete ruptures leave joints vulnerable to shifting.
Chronic overuse—common in runners or laborers—wears down tissues gradually. Repeated stress on the patellar tendon or meniscus erodes their shock-absorbing capacity. This creates micro-tears that accumulate over months, often unnoticed until instability becomes pronounced.
| Cause | Common Scenarios | Ligaments Affected | Cartilage Impact |
|---|---|---|---|
| Traumatic | ACL rupture during skiing | ACL, MCL | Meniscus tear |
| Overuse | Patellar tendinitis in runners | Patellar tendon | Articular wear |
The Role of Ligament Tears and Cartilage Damage
When ligaments fail to hold bones in alignment, adjacent cartilage bears uneven pressure. The menisci—crescent-shaped pads—may fray or split under abnormal friction. Left untreated, this cycle accelerates joint degeneration.
Early intervention breaks this pattern. Therapies like bracing or targeted strengthening redistribute forces properly. Addressing partial tears promptly prevents complete ruptures and preserves long-term mobility.
Non-Surgical Treatment Approaches for Knee Recovery
Many patients regain stability without invasive procedures through carefully structured protocols. Early intervention with evidence-based methods can significantly improve outcomes while minimizing downtime.
Rest, Ice, Compression, and Elevation (RICE) Techniques
The RICE method remains foundational for acute care. Here’s how it works:
- Rest: Pausing activities prevents further tissue stress
- Ice: 15-minute cold packs reduce inflammation
- Compression: Elastic wraps limit fluid buildup
- Elevation: Keeping the leg raised above heart level improves drainage
This approach tackles swelling and discomfort within the first 72 hours. Patients often notice improved mobility within days when combining RICE with proper bracing.
Structured physical therapy typically follows initial recovery. Therapists design programs emphasizing quadriceps activation and balance drills. Resistance bands and bodyweight movements rebuild strength gradually.
Three principles guide success:
- Starting exercises within pain-free ranges
- Progressing intensity weekly
- Monitoring joint response through functional tests
Consistent application of these strategies helps 78% of patients avoid surgery, according to recent studies. Always consult specialists to tailor plans for your unique needs.
Surgical Options and Considerations for Knee Rehabilitation
When non-surgical methods don’t restore stability, advanced procedures become the bridge to regained mobility. Decisions hinge on precise diagnostics—like MRI scans—that reveal torn fibers or cartilage erosion invisible during physical exams.
When Surgery Becomes Essential
Surgeons typically recommend intervention if:
- Persistent buckling occurs despite 3+ months of therapy
- Multiple ligaments are torn (e.g., ACL + MCL)
- Imaging confirms complete tendon ruptures
Common procedures include:
- ACL reconstruction: Replaces torn fibers with grafts
- Meniscus repair: Stitches damaged cartilage
- Osteotomy: Realigns bones to reduce joint pressure
| Procedure | Best For | Recovery Time | Success Rate |
|---|---|---|---|
| Partial Meniscectomy | Localized cartilage tears | 6-8 weeks | 85% |
| Full ACL Reconstruction | Complete ligament tears | 6-9 months | 92% |
“Modern minimally invasive techniques reduce tissue damage, allowing 73% of patients to resume light activities within 4 weeks.”
While surgery carries risks like infection or blood clots, benefits often outweigh drawbacks for active individuals. Post-op rehab—starting within days—is critical. Structured physiotherapy rebuilds strength while protecting healing tissues.
Data shows combining accurate diagnostics with personalized surgical plans yields optimal outcomes. For those facing persistent limitations, these interventions restore confidence in movement.
The Role of Rehabilitation and Strengthening Exercises
Restoring joint function demands more than passive recovery—it requires active, structured rehabilitation. We prioritize evidence-based methods that rebuild strength and flexibility while preventing future issues. Tailored programs adapt to individual progress, ensuring each phase of healing receives focused attention.
Effective Physical Therapy Methods
Specialists often begin with neuromuscular re-education to retrain muscles and improve coordination. Balance drills using wobble boards challenge stabilizing muscles, while resistance bands rebuild functional strength. Manual therapy techniques like soft tissue mobilization reduce scar tissue adhesion, enhancing mobility.
Milestones guide progress:
- Weeks 1-4: Focus on reducing swelling and restoring basic range of motion
- Weeks 5-8: Introduce weight-bearing exercises and proprioceptive training
- Months 3-6: Transition to sport-specific movements or advanced stability challenges
Key Exercises to Improve Range of Motion
Heel slides and seated leg extensions gently increase flexibility without strain. Step-ups onto low platforms strengthen quadriceps while promoting proper alignment. Wall squats with a stability ball build endurance in critical support muscles.
Consistency transforms recovery. Patients adhering to daily 15-minute sessions report 40% faster improvement in joint control compared to sporadic efforts. Pairing clinic visits with home routines creates compounding benefits, turning gradual gains into lasting stability.
Preventing Future Knee Instability and Maintaining Joint Health
Future-proofing your mobility requires more than just recovery—it demands foresight. Strategic habits built today can shield against tomorrow’s setbacks. Let’s explore how small, consistent choices create lasting resilience.
Proactive Strategies Before and After Injury
Weight management plays a crucial role—every pound lost reduces joint stress by four times during movement. Low-impact activities like swimming or cycling maintain fitness without straining vulnerable tissues. For athletes, mastering proper landing mechanics cuts injury risk by 53%, according to sports medicine studies.
Consider these evidence-backed practices:
- Prehabilitation programs: Tailored exercises address muscle imbalances before they cause issues
- Protective gear: Sport-specific braces stabilize during high-intensity movements
- Movement audits: Physical therapists analyze gait patterns to correct harmful techniques
Regular strength training remains non-negotiable. Focus on hamstrings and glutes—often neglected muscles that crucially support joint alignment. Our comprehensive treatment guide details how combining these methods with professional care maximizes results.
Schedule biannual mobility assessments, especially if you’re active. Early detection of subtle changes allows quick adjustments—whether modifying workouts or updating physical therapy routines. Remember: prevention isn’t about avoiding life; it’s about designing a body ready for it.
Final Steps for a Secure and Active Lifestyle
Progress begins when structured plans meet daily dedication. Whether managing recovery through non-surgical methods or post-op rehabilitation, consistency transforms temporary fixes into lasting results. Most patients see improved stability within 6-8 weeks when combining clinical guidance with home exercises.
Successful outcomes rely on three principles:
Early diagnosis pinpoints root causes, while personalized treatment addresses them. Regular therapy sessions rebuild strength gradually—starting with low-impact movements before advancing to sport-specific activities. Ongoing commitment from individuals ensures these gains endure.
Lifestyle adjustments play equal roles. Choosing joint-friendly exercises like cycling protects healing tissues. Maintaining healthy weight reduces strain, letting muscles work efficiently. People who track progress through mobility journals often stay motivated through plateaus.
Recovery isn’t linear, but each step forward matters. Trust the process, celebrate small wins, and lean on professional support when needed. With patience and persistence, confident movement becomes your new normal.
