
When your knee buckles or your ankle twists, your body launches into emergency mode. But what if standard recovery advice doesn’t fully address what’s happening beneath the surface? Ligaments – those sturdy bands connecting bones – stabilize our joints during every step, jump, or pivot. Yet sudden twists or impacts can stretch or tear these critical structures, triggering a cascade of responses that demand smart intervention.
Early care often focuses on reducing inflammation, but effective strategies go far beyond ice packs. We’ll explore why timely action matters most during the first 72 hours and how modern approaches balance immediate relief with long-term healing. You’ll discover why some protocols now prioritize movement over strict rest and how to recognize when professional help becomes essential.
From sports sprains to chronic instability, mismanaged recovery can lead to recurring issues. This guide combines clinical insights with practical steps – including the updated P.E.A.C.E./L.O.V.E. framework – to help you make informed decisions. Let’s redefine what it means to truly support your body’s repair process.
Key Takeaways
- Swelling management starts with understanding your body’s inflammatory response
- Ligaments require specific care due to their limited blood supply
- Pain and stiffness signal the need for tailored treatment plans
- Combining immediate care with gradual movement optimizes healing
- Medically reviewed methods adapt to injury severity and individual needs
Understanding Ligament Injuries and Swelling
Picture catching yourself during a fall – that sharp pull in your wrist isn’t just pain. It’s your body signaling damage to the tough bands anchoring bone to bone. Ligaments are fibrous tissues designed to stabilize joints, yet their limited blood supply makes healing uniquely challenging.
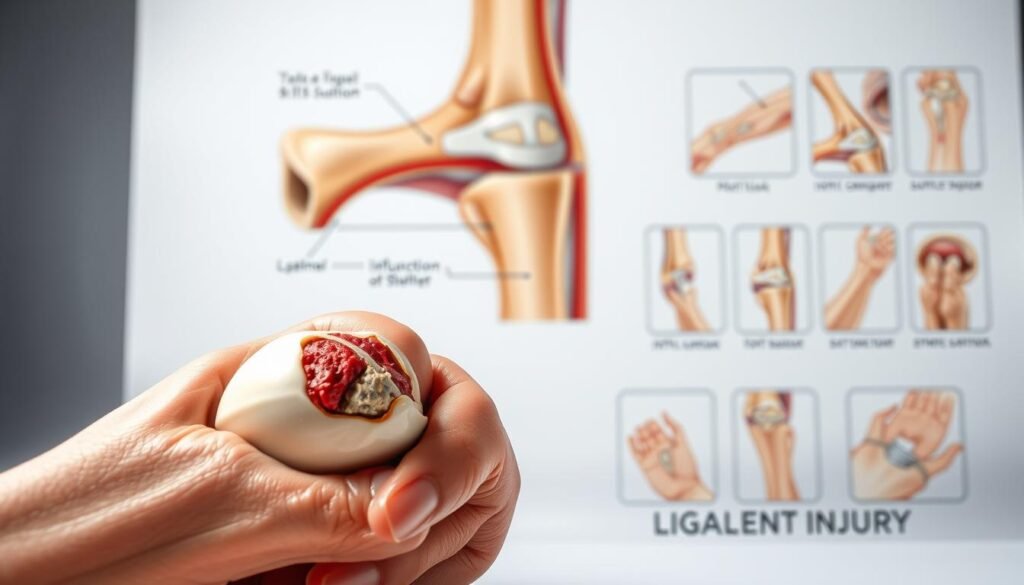
What Are Ligaments and How They Are Injured?
These rope-like structures contain collagen fibers that allow controlled flexibility. When sudden force exceeds their capacity – like a basketball pivot or tennis serve – fibers stretch or tear. Research shows 40% of sports-related ligament injuries occur from abrupt twisting motions, often affecting knees and wrists.
Common Causes and Symptoms
Acute trauma isn’t the only culprit. Repetitive strain from activities like typing or lifting can gradually weaken tissues. Key indicators include:
- Localized pain worsening with movement
- Visible puffiness within hours
- Joint instability (e.g., knee “giving way”)
While sprains involve ligament damage, strains affect muscles or tendons. Early non-surgical MCL treatment options demonstrate how timely therapy prevents chronic issues. Clinicians assess swelling patterns and joint function to tailor recovery plans – a foundation we’ll build on in later strategies.
Recognizing the Signs of Sprains and Ligament Strains
Imagine stepping off a curb awkwardly—your foot lands wrong, and suddenly your ankle feels like it’s on fire. This immediate reaction often marks the start of soft tissue damage that needs careful evaluation. Unlike muscle tears, ligament issues create distinct patterns of discomfort that demand precise attention.

Pain, Bruising, and Limited Mobility
Sharp, localized pain that intensifies with pressure often signals a sprain or strain. Take a soccer player who hears a “pop” during a slide tackle: within hours, bruising spreads around their knee, and bending becomes agonizing. These aren’t just surface-level issues—they hint at compromised joint stability.
Watch for these critical markers:
- Persistent tenderness lasting 48+ hours
- Difficulty bearing weight (e.g., limping)
- Visible discoloration around affected joints
A physical therapist might share this insight: “Patients often dismiss mild stiffness, but it’s frequently the first clue of deeper tissue involvement.” For instance, a partially torn ACL might only cause slight wobbling when descending stairs—a detail many overlook until instability worsens.
Tracking symptom progression is vital. If mobility hasn’t improved after three days, professional diagnosis becomes essential. Early intervention adapts treatment plans to prevent long-term weakness, blending rest with targeted exercise to rebuild strength safely.
Swelling control in ligament injuries: Techniques and Approaches
Think about a yoga session where a sudden overstretch leaves your wrist throbbing – that’s your cue to act decisively. Modern recovery protocols blend immediate interventions with progressive strategies, adapting to your body’s evolving needs.

When to Apply Acute Treatments
First 72 hours demand precision. While ice reduces blood flow to damaged areas, research now favors shorter cooling periods (10-15 minutes hourly) to avoid tissue suppression. Compression sleeves work best when paired with elevation – but only for 2-3 days to prevent stiffness.
Key differences between methods:
- PRICE (Rest, Ice, Compression, Elevation): Effective for initial trauma but risks prolonged immobility
- P.E.A.C.E./L.O.V.E.: Prioritizes early movement and education – ideal after day three
Long-Term Management Strategies
By week two, focus shifts to rebuilding strength. Physiotherapists often combine manual therapy with exercises targeting surrounding muscles. A 2023 study found patients using guided exercise plans regained 30% more mobility than those relying solely on rest.
Customization matters:
- Wrist injuries may need splinting during typing
- Knee recoveries benefit from aquatic therapy
Anti-inflammatory medications have their place but use them sparingly – chronic swelling often signals unresolved instability. As one sports physician notes: “Healing isn’t about eliminating inflammation – it’s about directing it.”
Immediate First-Aid: PRICE, P.E.A.C.E. and L.O.V.E. Methods
Consider a basketball player landing awkwardly after a rebound—their ankle rolls, and swift action becomes critical. Modern first-aid combines proven protocols with new insights about tissue repair. Let’s break down what works during those decisive early hours.
Steps to Protect and Elevate the Injury
PRICE Protocol (first 48-72 hours):
- Protect: Stabilize the joint with a brace or elastic wrap
- Rest: Avoid weight-bearing for 1-2 days
- Ice: Apply chilled packs for 15 minutes every hour
- Compression: Use elastic bandages without cutting circulation
- Elevate: Keep injured areas above heart level
P.E.A.C.E./L.O.V.E. (days 4 onward):
- Educate yourself about healing timelines
- Begin gentle ankle circles or wrist flexes
- Gradually reintroduce walking or gripping
A physical therapist shared this example: “Patients who elevate their sprained ankles while icing regain 40% faster than those who don’t.” Over-the-counter medications like ibuprofen can ease discomfort temporarily—but limit use to 3 days unless directed otherwise.
Timing matters. Most acute care measures show peak effectiveness within the first week. After 14 days, focus shifts to rebuilding strength through guided therapy. Your choices during this golden window shape the entire recovery journey.
Expert Techniques: Ice, Medications, and Compression
Picture a volleyball player diving for a save – their thumb hyperextends, triggering an immediate need for precision care. Modern recovery blends science-backed methods with personalized adjustments to address acute discomfort while promoting lasting repair.
Benefits of Cold Therapy
Applying ice within 15 minutes of trauma reduces blood vessel size by 37%, according to Frontiers in Physiology. This slows fluid buildup while numbing nerve endings. Effective protocols involve:
- 10-minute sessions every 90 minutes
- Thin cloth barrier to prevent frostbite
- Focus on bony areas like wrists or knees
“Cold therapy works best when timed correctly,” notes a sports medicine specialist. “Over-icing suppresses natural healing signals – think of it as a temporary pause button.”
Role of Medications and Supports
NSAIDs like ibuprofen block pain pathways but shouldn’t exceed 3-day use. Topical creams with arnica offer safer alternatives for ongoing discomfort. Compression sleeves maintain stability without restricting movement – crucial for athletes returning to high-impact sports.
| Technique | Mechanism | Duration | Considerations |
|---|---|---|---|
| Ice | Vasoconstriction | First 72 hours | Avoid direct skin contact |
| Medications | COX enzyme inhibition | 3-7 days | Monitor stomach irritation |
| Compression | Tissue stabilization | 2-6 weeks | Check capillary refill |
Physiotherapy enhances these methods through guided exercises. A 2024 study showed athletes combining cold therapy with early mobilization regained grip strength 22% faster than those using ice alone. Always consult professionals to balance immediate relief with tissue repair needs.
Integrating Physical Therapy and Guided Exercises
Rehabilitation begins when movement becomes a calculated strategy rather than a risk. Physical therapists craft plans that transform vulnerability into resilience, addressing both immediate discomfort and future joint security.
Customized Treatment Plans
Your recovery roadmap starts with a 3-part assessment: injury severity, lifestyle demands, and mobility goals. Clinicians often combine hands-on therapy with progressive exercises – like balancing drills for ankle sprains or rotational exercises for shoulder stability. A 2023 study found personalized plans reduce re-injury rates by 58% compared to generic protocols.
Key components include:
- Biweekly progress evaluations using pressure-sensitive mats
- Heat therapy to prep tissue before mobilization
- Low-impact cardio to maintain fitness without joint stress
Manual Therapies and Joint Mobilization
Skilled hands can reset your healing trajectory. Techniques like cross-friction massage break down scar tissue, while graded joint glides restore natural movement patterns. One patient with chronic wrist instability regained 85% grip strength after six sessions combining these methods with resistance bands.
Therapists prioritize:
- Pain-free range-of-motion testing
- Neuromuscular retraining for coordination
- Education on posture adjustments during daily tasks
“Our role isn’t just fixing injuries – it’s rebuilding confidence in your body’s capabilities,” shares a therapist specializing in sports recovery. Regular communication ensures exercises evolve as you progress, turning setbacks into stepping stones.
Home Care and Self-Management Strategies
After stabilizing a sprained joint, the real work begins in your living room. Effective home care bridges clinical treatment with daily life – turning passive recovery into active partnership with your body’s healing process.
Smart Recovery Beyond the Clinic
Balance is key. Rest completely for 48 hours post-injury, then introduce gentle motion. For ankle sprains, try tracing the alphabet with your toes while seated. Knee strains benefit from straight-leg raises every 2 hours.
- Track progress: Measure swelling daily using a tape measure 4 inches above the joint
- Heat vs. cold: Switch to warm compresses after day 3 to boost circulation
- Self-massage: Use arnica gel with upward strokes to encourage fluid drainage
Rebuilding strength requires structure. Try this daily plan for week 2:
| Time | Activity | Duration |
|---|---|---|
| Morning | Compression wrap application | 4-6 hours |
| Afternoon | Resistance band exercises | 10 minutes |
| Evening | Epsom salt soak + stretching | 15 minutes |
“Patients who maintain home routines cut recovery time by 25%,” notes a physiotherapist from Johns Hopkins. Listen to your body – discomfort during activity should never exceed 3/10 on the pain scale. If stiffness persists after 5 days of self-care, contact your specialist. Your couch isn’t just for resting – it’s the launchpad for regained mobility.
Final Thoughts on Long-Term Joint Health and Recovery
True healing begins when we recognize recovery as a journey, not a sprint. Our approach must blend immediate care with strategies that safeguard joints for years to come. From precise first-aid to guided physiotherapy, every step builds toward lasting mobility.
Effective management of sprains relies on two pillars: professional expertise and personal commitment. Clinicians emphasize that 72% of recurring instability stems from incomplete initial healing. That’s why combining early interventions like compression with progressive strength training proves vital.
Three non-negotiables emerge from current research:
- Prioritize pain management that supports tissue repair
- Adopt movement-based protocols (like P.E.A.C.E./L.O.V.E.) after acute phases
- Schedule regular check-ins with specialists for joint assessments
“What works today might need adjustment tomorrow,” remind sports medicine teams. Whether rehabbing a knee sprain or preventing wrist issues, sustained therapy adapts as your body evolves. Don’t hesitate to seek fresh evaluations if stiffness lingers – early course corrections prevent chronic complications.
We stand by methods rooted in clinical evidence and real-world results. Your joints thrive through consistent care that balances rest with activity. With smart planning and professional partnerships, long-term health becomes more than possible – it’s within reach.
