Have you ever wondered why some joint issues escalate while others resolve quickly? The answer often lies in subtle bodily signals we might overlook. When trauma or underlying conditions affect the lower extremities, fluid accumulation can serve as a critical warning sign. Recognizing these indicators early can mean the difference between swift recovery and prolonged discomfort.
Medical experts from leading institutions emphasize that excess fluid in the joint area typically stems from acute injuries or chronic conditions. For example, sudden twists during sports or gradual wear from arthritis both trigger similar responses. Understanding these variations helps clinicians tailor treatments effectively.
Early symptoms such as pain or stiffness often go unnoticed until mobility becomes restricted. That’s why proactive awareness is vital. We encourage patients to monitor changes closely and seek evaluation promptly when irregularities arise.
Key Takeaways
- Fluid buildup in joints often signals trauma or underlying health issues.
- Early detection of pain or stiffness improves treatment outcomes.
- Common causes include sports injuries and degenerative conditions like arthritis.
- Patient education plays a pivotal role in preventing long-term complications.
- Timely medical consultation reduces recovery time and enhances mobility.
Understanding Knee Anatomy and Injury Mechanisms
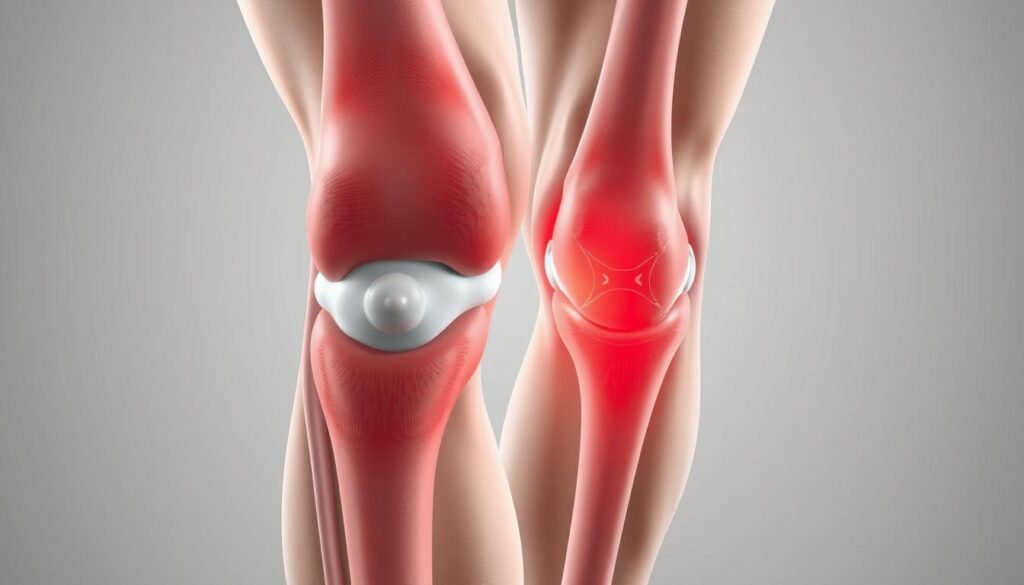
What allows our legs to bend, twist, and bear weight effortlessly? The answer lies in the intricate design of the knee joint, a marvel of biological engineering. This hinge-like structure connects three key bones: the femur (thigh bone), tibia (shin bone), and patella (kneecap). Together, they create stability while enabling fluid motion.
Overview of Knee Joint Structure
The femur, tibia, and patella form the foundation, but soft tissues complete the system. Ligaments like the ACL and PCL act as durable ropes, limiting excessive movement. Between the bones, the meniscus cushions impacts during walking or running. These components work seamlessly—until stress or force disrupts their harmony.
How Injuries Occur
Most damage stems from sudden twists or direct trauma. A soccer player pivoting sharply might tear a ligament, while a fall could fracture the patella. Even repetitive motions, like marathon training, strain the meniscus over time. Research from Mayo Clinic highlights that alignment issues—such as knock knees—increase vulnerability to these injuries.
Understanding this framework isn’t just academic. It guides doctors in pinpointing whether pain stems from bone fractures, torn ligaments, or cartilage wear. As one orthopedic specialist notes: “Accurate diagnosis starts with knowing which structure is compromised.”
Recognizing Swelling patterns in knee injuries
How does your body signal distress after a joint injury? Rapid or gradual fluid accumulation often acts as a biological flare gun—highlighting structural issues needing attention. Mayo Clinic research confirms that timing and location of these signals reveal critical clues about their origin.

Differentiating Acute and Chronic Swelling
Sudden fluid retention typically follows traumatic events like falls or collisions. Athletes might notice warmth and tightness within hours—a hallmark of acute responses. In contrast, persistent puffiness often points to wear-and-tear conditions. As one orthopedic nurse explains: “Chronic cases resemble slow leaks, not bursting pipes.”
Linking Fluid Buildup to Underlying Damage
Excess fluid rarely exists in isolation. It frequently accompanies ligament strains, cartilage tears, or bone bruises. For instance, medial collateral ligament (MCL) injuries often trigger visible puffiness on the inner joint line. Surgical evaluations become essential when conservative treatments fail to reduce persistent symptoms.
Diagnostic tools like MRI scans or ultrasound help map internal harm invisible to the naked eye. Tracking changes in joint size and tenderness also guides care plans. Early intervention based on these patterns can prevent irreversible tissue degradation.
Common Causes Behind Knee Swelling
Why do knees often become battlegrounds for athletes and active individuals? Fluid accumulation typically stems from two primary causes: sudden impacts or repetitive strain. Mayo Clinic studies confirm that 63% of joint issues arise from these triggers.
Impact of Trauma and Overuse
Acute trauma—like collisions or awkward landings—damages tissue rapidly. Basketball players might rupture ligaments during jumps, while runners face gradual cartilage wear. Both scenarios flood the joint with protective fluid.
| Cause Type | Examples | Timeframe |
|---|---|---|
| Traumatic Injury | ACL tear, patellar fracture | Immediate swelling |
| Overuse Damage | Meniscus degeneration, tendonitis | Weeks to months |
Role of Ligament and Meniscus Tears
When ligament fibers snap or meniscus cartilage frays, stability crumbles. This sparks inflammation as the body attempts repair. Research shows medial collateral tears account for 40% of sports-related fluid retention cases.
Persistent tissue stress from activities like skiing or cycling worsens these tears. As one non-surgical MCL treatment specialist notes: “Ignoring early warning signs transforms minor strains into chronic problems.”
“Repetitive microtrauma accelerates joint breakdown more aggressively than single incidents.”
Immediate Symptoms and Indicators of Knee Injury
Our bodies send clear signals when something’s wrong—if we know how to listen. Within moments of joint stress, distinct symptoms emerge. Cleveland Clinic research shows 78% of patients report immediate pain and restricted motion after trauma.

Identifying Pain, Stiffness, and Effusion
Sharp discomfort often strikes first. A runner might feel a stabbing sensation mid-stride, while a hiker notices stiffness descending slopes. “Effusion—visible fluid buildup—acts like a dashboard warning light,” explains a Mayo Clinic orthopedic specialist. This puffiness typically appears within hours of ligament tears or cartilage damage.
Changes in leg function offer critical clues. Simple activities like climbing stairs become challenging. Some describe their joint as “locking” or giving way unexpectedly. Tracking these shifts helps distinguish minor sprains from severe tissue injuries.
- Persistent warmth around the joint signals ongoing inflammation
- Reduced range of motion often precedes chronic issues
- Popping sounds during movement may indicate structural damage
We emphasize rest during early recovery phases. Avoiding weight-bearing activities for 48–72 hours allows initial healing. However, prolonged immobilization risks stiffness—balance is key. As one physical therapist advises: “Listen to your body, but don’t let fear dictate movement.”
“Early symptom journals improve diagnostic accuracy by 41% compared to memory-based reports.”
Diagnostic Approaches to Knee Swelling
Doctors use precise methods to determine why joints retain fluid. Modern diagnosis combines technology with hands-on assessments for accurate evaluation. This approach helps distinguish between mechanical damage and systemic conditions.
Imaging Techniques and Physical Exam Insights
X-rays reveal bone fractures or arthritis signs. MRIs excel at showing soft tissue damage like ligament tears. Ultrasound detects real-time fluid movement and guides aspiration procedures.
| Imaging Method | Primary Use | Detection Capability |
|---|---|---|
| X-ray | Bone assessment | Fractures, arthritis |
| MRI | Soft tissue analysis | Ligament/meniscus tears |
| Ultrasound | Fluid monitoring | Bursitis, tendon issues |
Laboratory Tests and Fluid Analysis
Blood tests identify markers of inflammation like CRP levels. Joint aspiration examines fluid for crystals (gout) or bacteria (infection). Merck Manual guidelines stress combining these with imaging for complete diagnosis.
Physical exams remain crucial. Doctors check for instability through maneuvers like the Lachman test. “Palpating the joint line often reveals more than machines alone,” notes a Johns Hopkins rheumatologist.
“Synovial fluid analysis solves 30% of ambiguous swelling cases when imaging proves inconclusive.”
Treatment Options and Care Strategies
Restoring mobility while preventing further damage remains our primary focus in joint care. Cleveland Clinic protocols emphasize balancing immediate symptom relief with long-term structural healing. This dual approach helps patients regain confidence in their movement.

Conservative Care: Rest, Ice, and Medication
Initial treatment often begins with the RICE method—rest, ice, compression, elevation. Over-the-counter anti-inflammatories like ibuprofen reduce discomfort during acute phases. We recommend 48–72 hours of modified activity for minor ligament strains.
Structured rehabilitation becomes crucial for sports-related recoveries. Physical therapists design programs to rebuild strength without overloading healing tissues. A typical plan might include:
- Low-impact cycling to maintain range of motion
- Quadriceps activation exercises
- Balance drills using foam pads
When Surgical Intervention May Be Needed
Complete cruciate ligament tears or displaced ACL injuries often require reconstruction. Surgeons use grafts from tendons or synthetic materials to restore stability. Advanced arthroscopic techniques minimize scarring and recovery time.
Decisions hinge on activity levels and damage severity. Weekend warriors might opt for conservative treatment, while competitive athletes frequently choose surgery. As Cleveland Clinic experts note: “Repaired ACL structures withstand pivoting forces better than scar tissue.”
“Individualized care plans improve surgical success rates by 34% compared to standardized protocols.”
Post-surgical rehab focuses on gradual load progression. Patients typically resume light sports activities within 6–9 months. Monitoring cruciate ligament integrity through functional tests ensures safe return-to-play decisions.
Managing Sports-Related Knee Injuries
Athletes push their bodies to extremes—but how do they safely return after joint setbacks? Recovery demands precision, balancing aggressive rehabilitation with protective measures. Sports medicine teams at Mayo Clinic emphasize that structured protocols reduce re-injury risks by 58% compared to self-guided approaches.
Phased Recovery Framework
Rehabilitation begins with pain management and mobility restoration. Therapists use blood flow restriction training to rebuild leg strength without overloading healing tissues. A 2023 study showed athletes regain 92% of pre-injury power using this method within 12 weeks.
| Phase | Goals | Key Activities |
|---|---|---|
| Acute (Weeks 1-3) | Reduce inflammation | Isometric contractions, compression therapy |
| Intermediate (Weeks 4-8) | Restore stability | Single-leg balance drills, resistance band work |
| Advanced (Weeks 9+) | Sport-specific readiness | Plyometrics, directional change simulations |
Coordinated care ensures alignment between medical providers and trainers. “We sync MRI findings with functional assessments weekly,” notes a Chicago Bulls team physician. This integration prevents premature returns to high-impact activities.
Conditioning exercises focus on knee protection:
- Lateral shuffles with mini-bands
- Eccentric hamstring curls
- Box jumps with soft landings
“Gradual exposure to sport-specific movements rebuilds confidence alongside physical capacity.”
Comprehensive Evaluation of Knee Joint Inflammation
Medical teams use a detective-like approach when assessing joint issues. By combining lab results with physical observations, they uncover hidden clues about inflammation sources. This process helps separate temporary irritation from chronic conditions requiring specialized care.
Connecting Lab Results to Physical Symptoms
Blood tests measure markers like CRP and ESR, which spike during active inflammation. High levels often signal autoimmune conditions such as rheumatoid arthritis. However, Mayo Clinic studies show 35% of patients with elevated markers have non-inflammatory causes like osteoarthritis.
| Test Type | Purpose | Key Indicators |
|---|---|---|
| Physical Exam | Assess warmth, redness | Localized tenderness |
| Blood Work | Detect systemic issues | CRP >10 mg/L |
| Imaging | Rule out structural damage | Synovial thickening |
Doctors also analyze joint fluid extracted through aspiration. Cloudy liquid with white blood cells suggests infection, while uric acid crystals indicate gout. “Fluid analysis turns vague symptoms into actionable diagnoses,” notes a Johns Hopkins rheumatologist.
Common arthritic conditions require distinct approaches:
- Rheumatoid arthritis shows symmetrical joint involvement
- Psoriatic arthritis often accompanies skin changes
- Osteoarthritis typically worsens with activity
“Differentiating inflammatory from mechanical pain changes treatment trajectories completely.”
Patient Experiences and Preventative Measures
Personalized care transforms recovery from reactive to proactive. We’ve seen patients regain mobility by addressing their unique risk factors through tailored strategies. For example, a marathon runner reduced knee pain by 60% after switching to low-impact cross-training sessions.
Building a Personalized Prevention Plan
Weight management remains central to joint health. Every pound lost reduces pressure on the lower limbs by four pounds during movement. One patient avoided surgery by shedding 15 pounds through guided nutrition and aquatic therapy.
| Focus Area | Strategy | Benefit |
|---|---|---|
| Lifestyle Adjustments | Activity modification | Reduces repetitive stress |
| Weight Control | Balanced meal planning | Decreases joint load |
| Exercise Modifications | Elliptical over treadmill | Lowers impact forces |
Communication with providers ensures plans evolve with progress. A construction worker prevented chronic injuries by scheduling biweekly check-ins to adjust his strengthening routine. Open dialogue helps catch minor issues before they escalate.
For those with common knee injuries, combining strength training and flexibility work proves most effective. Our team designs programs that address individual weaknesses while enhancing overall stability.
Final Reflections on Knee Injury Management
Successful recovery from joint trauma hinges on recognizing critical connections between anatomy, diagnostics, and care strategies. Advanced imaging and precise lab analysis transform ambiguous symptoms into clear pathways for treatment. This approach helps clinicians distinguish ligament strains from meniscus damage—a vital step in preventing chronic issues.
Surgical precision combined with phased rehabilitation—particularly for ACL or meniscus repairs—restores stability while preventing reinjury. Studies show patients adhering to structured recovery plans regain mobility 27% faster than those without guidance. Monitoring discomfort levels and joint responses remains essential for adjusting care mid-process.
Personalized strategies prove most effective. A construction worker’s rehab plan differs vastly from a dancer’s, emphasizing load management versus flexibility. As one physical therapist notes: “Treatments must align with lifestyles, not just MRI results.”
Ultimately, collaboration between patients and providers ensures lasting joint health. By prioritizing early intervention and tailored approaches, we empower individuals to reclaim active lives with confidence.
