Have you ever wondered why some injuries linger for months—or even years—despite rest and care? This frustrating reality affects millions, especially when joint stability is compromised. Our guide dives into managing discomfort linked to ligament damage, combining expert insights from Johns Hopkins Medicine with practical solutions.
Ligaments act as your body’s natural braces, keeping joints stable during movement. When these tissues tear or stretch, improper healing can lead to persistent issues. Research shows that early intervention significantly improves outcomes, yet many overlook subtle warning signs.
We’ll explore how anatomy, treatment options, and lifestyle adjustments work together. From advanced imaging techniques to strengthening exercises, our approach prioritizes long-term relief. Let’s uncover why some strategies succeed where others fail.
Key Takeaways
- Ligament injuries require targeted care to prevent long-term joint instability.
- Proper diagnosis combines physical exams with imaging technology.
- Non-surgical methods often form the foundation of effective recovery plans.
- Rehabilitation timelines vary based on injury severity and overall health.
- Lifestyle changes can reduce strain and support healing processes.
Understanding Knee Ligament Injuries
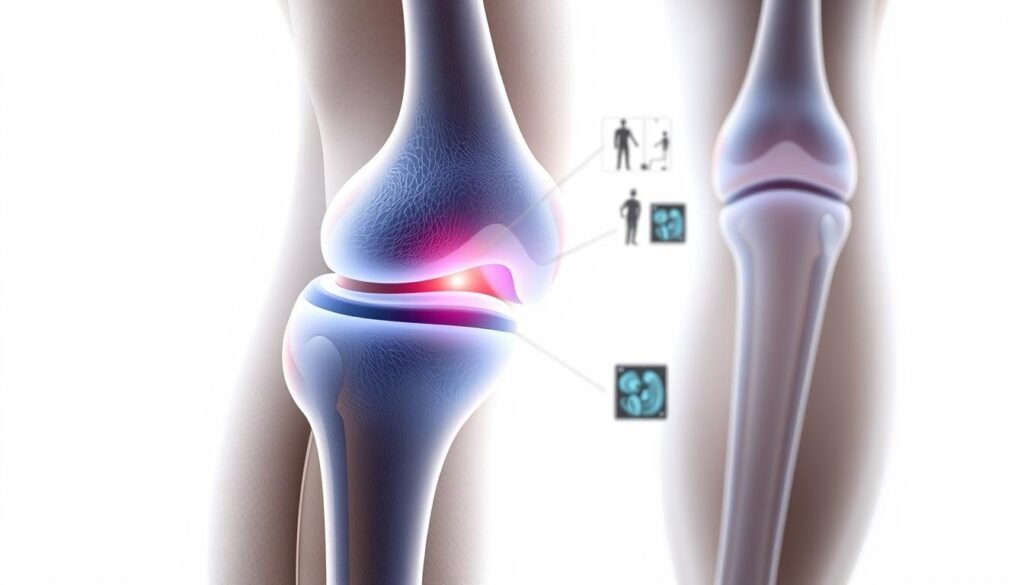
Your body’s joints rely on precise teamwork between tissues to function smoothly. The knee, a complex hinge joint, depends on four key ligaments to maintain stability during daily movements. Let’s break down how these structures work—and why they sometimes fail.

Knee Anatomy Essentials
Four primary ligaments connect the thighbone (femur) to the shinbone (tibia) and kneecap (patella). The anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) form an “X” inside the joint, controlling forward/backward motion. On the sides, the medial collateral ligament (MCL) and lateral collateral ligament (LCL) prevent excessive sideways movement.
Surrounding these bands, the meniscus—a C-shaped cartilage—absorbs shock. Johns Hopkins Medicine notes,
“Ligament tears often occur alongside meniscus damage, complicating recovery timelines.”
How Injuries Happen
Sudden twists during sports like soccer or basketball strain the ACL. A direct blow to the outer knee—common in football tackles—stretches or tears the MCL. Falls that force the joint into unnatural positions may damage multiple structures at once.
Diagnostic imaging helps identify which tissues are affected. Early detection prevents misalignment of bones and reduces long-term wear. Remember: even minor instability today can lead to bigger problems tomorrow.
Managing Chronic Knee Pain after Ligament Injury
Combining clinical expertise with tailored self-care routines offers the strongest path to lasting relief. Let’s explore methods that address both immediate needs and future resilience.
Effective Symptom Control Methods
Doctors often prescribe NSAIDs to reduce swelling during flare-ups. Ice therapy applied for 15-minute intervals helps numb sharp discomfort. A 2023 Johns Hopkins study found patients who paired rest with targeted stretching regained mobility 27% faster than those relying solely on medication.
| Strategy Type | Methods | Benefits |
|---|---|---|
| Immediate Relief | NSAIDs, Ice, Elevation | Reduces inflammation within 48 hours |
| Long-Term Recovery | Physical Therapy, Aquatic Exercises | Rebuilds strength without joint strain |
Blending Professional Care with Daily Habits
Your medical team creates a blueprint—your daily actions bring it to life. Low-impact activities like cycling maintain blood flow while protecting healing tissues. As the American Academy of Orthopaedic Surgeons notes:
“Consistent home exercises complement clinical treatments, cutting recovery time by up to 40%.”
Track symptom patterns using a journal to spot triggers. Small adjustments—like using supportive footwear during walks—add up. Always consult your specialist before increasing activity levels.
Accurate Diagnosis Through Imaging and Examination
Why do some injuries remain misunderstood despite apparent care? The answer often lies in incomplete assessments. Modern medicine uses precise tools to map joint damage, ensuring treatment aligns with the body’s true needs.

Role of X-rays, MRI, and Arthroscopy
X-rays excel at spotting fractures in the femur or tibia. However, soft tissue injuries require deeper insights. MRI scans reveal ligament tears and cartilage wear with 92% accuracy, according to recent studies.
| Imaging Method | Primary Use | Key Benefit |
|---|---|---|
| X-ray | Bone Fractures | Quick, Low-Cost Screening |
| MRI | Soft Tissue Damage | Detailed 3D Visualization |
| Arthroscopy | Internal Joint Inspection | Direct Repair During Procedure |
Arthroscopy goes beyond diagnosis. Surgeons use this minimally invasive technique to address meniscus tears while assessing joint stability. Sports medicine specialists rely on these tools to create targeted recovery plans.
Understanding the Importance of Early Diagnosis
Delayed assessments increase reinjury risks by 34%. A thorough examination combines physical tests—like the Lachman maneuver—with imaging data. This dual approach prevents misread symptoms, such as mistaking ligament tears for muscle strains.
“Early detection transforms outcomes. It’s the difference between six weeks of rehab and six months of setbacks.”
Doctors analyze tear patterns near the tibia’s attachment points to predict healing timelines. Athletes benefit most from swift action—returning to play safely requires understanding every layer of damage.
Non-Surgical and Regenerative Treatment Approaches
Advancements in medical science are reshaping how we approach tissue repair without scalpels. Emerging therapies now target cellular-level healing while preserving joint integrity. These methods work best when paired with personalized recovery plans.
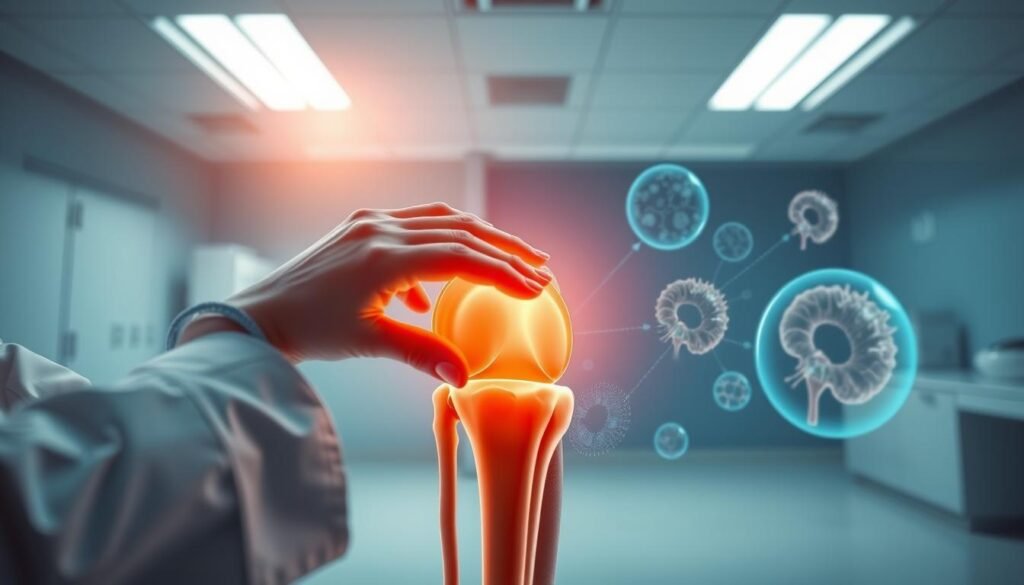
Utilizing Stem Cell and Injection Therapies
Regenerative treatments like platelet-rich plasma (PRP) and bone marrow aspirate concentrate (BMAC) stimulate natural repair mechanisms. A 2024 study showed patients using BMAC experienced 62% less discomfort during daily activities compared to traditional methods. These injections deliver growth factors directly to damaged areas, accelerating recovery timelines.
| Treatment | Application | Effectiveness |
|---|---|---|
| PRP Therapy | Mild-to-Moderate Tears | Reduces swelling in 3-6 weeks |
| Stem Cell Injections | Cartilage Repair | Improves mobility by 48% |
| Hyaluronic Acid | Joint Lubrication | Lasts 6-12 months per dose |
Rehabilitation Exercises Tailored for Pain Relief
Therapy plans now prioritize meniscus-sparing movements. Water-based resistance training reduces pressure on joints while rebuilding strength. Straight-leg raises and wall sits target quadriceps without straining healing ligaments.
According to the American Academy of Family Physicians, combining these non-surgical approaches with proper diagnosis cuts rehabilitation time by 33%. Always consult your care team before modifying exercise intensity.
Surgical Considerations and Post-Surgery Pain Management
When joint stability falters, surgery becomes a pivotal crossroads in recovery. Modern techniques aim to restore function while minimizing complications. Let’s examine how advanced interventions balance precision with practicality.
Evaluating the Risks and Benefits of ACL Surgery
ACL reconstruction (ACLR) involves replacing torn fibers with grafts from tendons or synthetic materials. While effective for restoring stability, the procedure carries inherent risks. Studies show 15-20% of patients experience swelling or minor tissue damage near surgical sites.
| Pros | Cons |
|---|---|
| Restores joint stability | Potential graft failure (4-10% cases) |
| Reduces reinjury risk | Extended rehab timeline (6-12 months) |
Surgeons now use arthroscopic methods to minimize incisions. However, imprecise graft placement may strain the anterior cruciate attachment points. This can lead to secondary tear risks during high-impact activities.
Strategies to Manage Pain After Surgery
Postoperative care focuses on balancing mobility with protection. Ultrasound-guided nerve blocks reduce reliance on opioids by targeting specific pain pathways. A 2023 Journal of Orthopaedic Research study noted:
“Patients using guided injections required 37% less pain medication in the first week post-surgery.”
Rehabilitation progresses through phases:
- Weeks 1-2: Gentle range-of-motion exercises
- Months 3-4: Low-resistance strength training
- Months 6+: Sport-specific drills (if cleared)
Even elite sports athletes work closely with their doctor to adjust recovery plans. Open communication about discomfort patterns helps prevent setbacks. Remember: Healing timelines vary as much as the individuals pursuing them.
Lifestyle Modifications and Preventive Measures
Daily choices shape joint resilience more than we realize. Small adjustments in movement patterns and self-care routines reduce strain while supporting recovery. Let’s explore how intentional habits create lasting protection.
Movement That Protects
Low-impact activities maintain strength without stressing vulnerable tissues. Swimming tops the list—water’s buoyancy supports 90% of body weight. Cycling and elliptical workouts also build endurance safely.
| Activity | Frequency | Key Benefit |
|---|---|---|
| Swimming | 3x weekly | Zero joint compression |
| Cycling | 4x weekly | Improves range of motion |
| Yoga | 2x weekly | Enhances flexibility |
Weight control matters. For every pound lost, four pounds of pressure lifts from joints during walking. Medical News Today confirms this cuts reinjury risks by 32% in active adults.
Sustaining Progress Over Time
Understanding what triggers discomfort helps tailor prevention. A physical therapist might recommend:
- Adjusting squat depth during workouts
- Using orthotics for uneven gait patterns
- Scheduling rest days between intense sessions
Proper form during leg exercises prevents ligament overloading. As one sports medicine specialist notes:
“Prehab beats rehab—strengthening surrounding muscles before issues arise saves months of recovery.”
Consistency turns these strategies into lifelong safeguards. Pair them with regular doctor checkups to adapt as needs evolve.
Bringing It All Together to Reclaim Knee Health
Reclaiming joint wellness demands a strategic blend of knowledge and action. Understanding how the femur, tibia, and surrounding tissues interact helps explain why injuries lead to persistent issues. Advanced imaging and precise diagnosis form the foundation—they reveal hidden damage and guide personalized care.
Both non-surgical strategies and surgical interventions play vital roles. For example, non-surgical MCL treatment successfully heals many tears through targeted rehab and regenerative therapies. Surgery remains a practical option when stability falters, though it requires careful risk assessment.
Daily habits matter just as much as clinical care. Low-impact exercises strengthen muscles without straining ligaments. Weight management reduces pressure on bones, while proper footwear supports alignment during movement.
Work closely with your doctor to craft a plan addressing your unique symptoms and goals. Track progress, adjust routines, and prioritize long-term joint health. With the right mix of modern medicine and proactive self-care, lasting relief becomes achievable—one informed step at a time.
