When it comes to MCL (medial collateral ligament) injuries, your age plays a crucial role in determining how quickly and effectively you’ll heal. Whether you’re a teenager with a sports injury or a senior who slipped on ice, understanding how age impacts MCL sprain healing time can help you set realistic expectations and optimize your recovery process. This comprehensive guide explores the biological reasons behind age-related healing variations, compares recovery timelines across different age groups, and provides actionable strategies to support your MCL healing journey.
Understanding MCL Injuries: A Quick Overview
The medial collateral ligament (MCL) connects the femur to the tibia on the inner side of the knee
The medial collateral ligament (MCL) is a broad, thick band that runs down the inner part of the knee, connecting the thigh bone (femur) to the shin bone (tibia). It primarily prevents the leg from extending too far inward while also helping to stabilize the knee joint during movement.
MCL tears are classified into three grades based on severity:
- Grade 1 (Mild): Minor stretching and microscopic tearing of the ligament fibers with minimal tenderness and pain.
- Grade 2 (Moderate): Partial tearing of the ligament with noticeable looseness in the knee joint, moderate pain, and some joint instability.
- Grade 3 (Severe): Complete tear of the ligament resulting in significant pain, swelling, and joint instability.
While the grade of the tear significantly influences recovery time, age is an equally important factor that affects how quickly and completely the MCL heals. Let’s explore why age makes such a difference in the healing process.
Biological Reasons for Age-Related Healing Variations
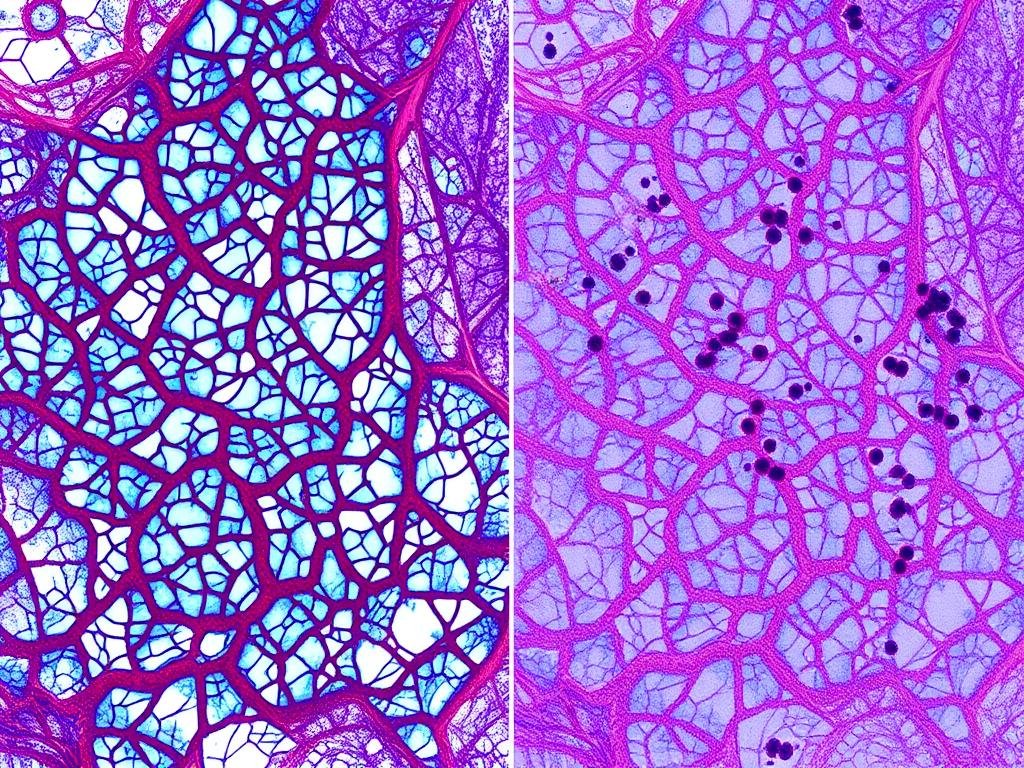
Microscopic comparison showing differences in collagen production between younger and older MCL tissue
Collagen Production and Quality
Collagen is the primary structural protein in ligaments, providing strength and elasticity. As we age, our bodies produce less collagen, and the quality of that collagen changes significantly:
- Younger individuals (under 40): Produce abundant, high-quality collagen with better cross-linking, resulting in stronger repair tissue.
- Middle-aged individuals (41-65): Experience a gradual decline in collagen production, with approximately 1-1.5% reduction per year after age 30.
- Seniors (65+): Produce significantly less collagen with poorer organizational structure, leading to weaker repair tissue that takes longer to form.
Blood Flow and Vascularization
Adequate blood supply is essential for delivering oxygen, nutrients, and healing factors to injured tissues:
- Adolescents and young adults: Have excellent blood flow to ligaments with robust vascular networks that quickly mobilize healing resources.
- Middle-aged adults: Experience moderate reduction in microcirculation to ligamentous tissues.
- Seniors: Often have significantly reduced blood flow due to vascular changes, atherosclerosis, and other age-related circulatory issues, slowing the delivery of healing components to the injured MCL.
Cellular Regeneration and Inflammatory Response
The body’s ability to generate new cells and regulate inflammation changes with age:
- Younger individuals: Have more efficient stem cell mobilization and higher numbers of mesenchymal stem cells that can differentiate into ligament cells.
- Older individuals: Experience reduced stem cell functionality and numbers, limiting regenerative capacity.
- Inflammatory response: Tends to be more efficient in younger people and more prolonged or dysregulated in older adults, potentially delaying the transition from inflammatory to proliferative healing phases.
Need Personalized Guidance for Your MCL Recovery?
Our sports medicine specialists can evaluate your specific injury and create an age-appropriate recovery plan to optimize your healing process.
Age-Based MCL Recovery Timelines: What to Expect
Comparative healing timelines for MCL sprains across different age groups
Recovery times for MCL injuries vary significantly based on both the grade of the tear and the patient’s age. The following table provides a comprehensive comparison of healing phases across different age groups:
| Healing Phase | Adolescents (12-18) | Young Adults (19-40) | Middle-Aged (41-65) | Seniors (65+) |
| Inflammatory Phase | 3-5 days | 5-7 days | 7-10 days | 10-14 days |
| Proliferative Phase | 5-14 days | 7-21 days | 14-28 days | 21-35 days |
| Remodeling Phase | 2-6 weeks | 3-8 weeks | 6-12 weeks | 8-16 weeks |
| Grade 1 MCL Recovery | 1-2 weeks | 1-3 weeks | 2-4 weeks | 3-5 weeks |
| Grade 2 MCL Recovery | 2-3 weeks | 3-4 weeks | 4-6 weeks | 6-8 weeks |
| Grade 3 MCL Recovery | 4-6 weeks | 5-7 weeks | 7-10 weeks | 10-16 weeks |
| Return to Sports/Full Activity | 4-8 weeks | 6-10 weeks | 8-14 weeks | 12-20 weeks |
Key Observations About Age and MCL Recovery
Adolescents (12-18)
Teenagers typically experience the fastest healing times due to their robust biological healing mechanisms. Their bodies have excellent blood supply to ligaments, optimal collagen production, and efficient cellular regeneration. However, compliance with treatment protocols can sometimes be an issue, and growth plate considerations may affect treatment approaches.

Adolescents often recover quickly but need proper guidance to ensure complete healing
Young Adults (19-40)
Young adults maintain excellent healing capacity while typically demonstrating better compliance with rehabilitation protocols. Their recovery is often straightforward with predictable timelines, though lifestyle factors like smoking, alcohol consumption, and nutrition can significantly impact healing efficiency. Work demands may sometimes interfere with optimal rest periods.

Young adults benefit from stationary bike exercises during MCL rehabilitation
Middle-Aged Adults (41-65)
Middle-aged individuals experience noticeably longer healing times due to declining collagen quality and reduced cellular regeneration. Comorbidities like diabetes, hypertension, or obesity can further extend recovery periods. However, this age group often demonstrates excellent compliance with treatment protocols and realistic expectations about recovery timelines.

Middle-aged adults may require more hands-on therapy to optimize MCL healing
Seniors (65+)
Seniors face the longest recovery times due to significantly reduced healing capacity. Decreased blood flow, diminished collagen production, and age-related comorbidities all contribute to extended healing periods. Balance and mobility issues may complicate rehabilitation, and modifications to standard protocols are often necessary to accommodate age-related limitations.

Seniors often require walking aids and modified protocols during MCL recovery
Get Your Age-Specific MCL Recovery Guide
Download our comprehensive guide with detailed recovery timelines, exercises, and nutrition recommendations tailored to your age group.
Age-Specific Treatment Adaptations for MCL Injuries

Different knee braces and supports may be recommended based on age and activity level
Treatment approaches for MCL injuries should be tailored to the patient’s age to optimize healing and functional outcomes. Here’s how treatment strategies differ across age groups:
Immobilization and Bracing
| Age Group | Bracing Approach | Duration | Special Considerations |
| Adolescents (12-18) | Functional hinged brace allowing controlled movement | Shorter periods (1-3 weeks depending on grade) | Growth plate protection; sports-specific bracing for return to play |
| Young Adults (19-40) | Functional bracing with progressive movement allowance | Standard protocol (2-4 weeks depending on grade) | Work accommodation; sports-specific return protocols |
| Middle-Aged (41-65) | More supportive bracing with gradual weaning | Extended periods (3-6 weeks depending on grade) | Comorbidity management; work ergonomics |
| Seniors (65+) | Maximum support bracing with easy application design | Longest duration (4-8 weeks depending on grade) | Fall prevention; ease of use; assistance with application |
Physical Therapy Modifications

Physical therapy approaches vary significantly based on patient age and healing capacity
Adolescents
- Higher intensity rehabilitation with faster progression
- Focus on neuromuscular control and proprioception
- Sport-specific training introduced earlier
- Growth plate-safe exercises
- Education on injury prevention crucial
Young Adults
- Standard progression protocols
- Balance between aggressive rehabilitation and adequate healing time
- Work-specific functional training
- Focus on preventing re-injury
- Strength training emphasized
Middle-Aged Adults
- More gradual progression through rehabilitation phases
- Additional focus on general conditioning
- Management of comorbidities during rehabilitation
- Emphasis on proper biomechanics
- Work-related modifications and ergonomics
Seniors
- Gentler, more supported exercises
- Significantly slower progression
- Balance and fall prevention integration
- Aquatic therapy often beneficial
- Focus on functional independence and activities of daily living
Medication and Supplementation Considerations
| Age Group | Pain Management | Recommended Supplements | Precautions |
| Adolescents | Conservative use of NSAIDs; acetaminophen preferred | Vitamin D, calcium, protein | Growth plate considerations; shorter NSAID courses |
| Young Adults | Standard NSAID protocols; short-term use | Vitamin C, protein, collagen peptides | Gastrointestinal effects of NSAIDs |
| Middle-Aged | Careful NSAID use; consider cyclooxygenase-2 inhibitors | Collagen, vitamin D, omega-3 fatty acids | Cardiovascular and renal considerations with NSAIDs |
| Seniors | Acetaminophen preferred; limited NSAID use | Vitamin D, calcium, collagen, protein | Medication interactions; renal function; fall risk with certain medications |
Age-Specific Recovery Tips for MCL Sprains
The RICE method (Rest, Ice, Compression, Elevation) remains important for all age groups
Recovery Tips for Adolescents (12-18)
1. Structured Activity Progression
Teenagers often rush back to sports too quickly. Create a clear, progressive return-to-play protocol with specific milestones that must be achieved before advancing to the next level of activity. Having concrete goals helps maintain compliance and prevents premature return.
2. Growth-Plate Safe Exercises
Work with a physical therapist familiar with adolescent athletes to ensure exercises don’t place undue stress on growth plates. Focus on closed-chain exercises that build strength without risking growth plate injuries, particularly important during peak growth periods.
3. Peer Support Systems
Connect recovering teens with peers who have successfully rehabilitated similar injuries. The social aspect of recovery is particularly important for adolescents, and seeing others who have successfully returned to sports provides motivation and realistic expectations.
Recovery Tips for Young Adults (19-40)
1. Work Accommodation Planning
Develop a specific plan for work modifications during recovery. This might include temporary desk arrangements, reduced standing/walking requirements, or modified duties. Having a clear plan helps prevent workplace reinjury and supports optimal healing.
2. Anti-inflammatory Nutrition
Adopt an anti-inflammatory diet rich in omega-3 fatty acids, antioxidants, and whole foods. Young adults have the metabolic capacity to significantly influence healing through nutrition. Minimize processed foods, alcohol, and sugar which can promote inflammation.
3. Sleep Optimization
Prioritize sleep quality and quantity, aiming for 7-9 hours of uninterrupted sleep. Growth hormone release during deep sleep is crucial for tissue repair. Create a consistent sleep schedule and optimize your sleep environment for maximum recovery benefit.
Recovery Tips for Middle-Aged Adults (41-65)
1. Comprehensive Conditioning
Focus on whole-body conditioning rather than isolated knee exercises alone. Middle-aged adults benefit from maintaining overall fitness during recovery, which supports MCL healing while preventing deconditioning of other systems that could slow return to function.
2. Comorbidity Management
Optimize management of any existing health conditions like diabetes, hypertension, or arthritis. Work with your primary care physician to ensure these conditions are well-controlled during recovery, as they can significantly impact healing timeframes.
3. Targeted Supplementation
Consider evidence-based supplements like vitamin D, collagen peptides, and glucosamine-chondroitin after consulting with your healthcare provider. These may help support connective tissue repair, particularly beneficial as natural production of these compounds declines with age.
Recovery Tips for Seniors (65+)
1. Fall Prevention Strategy
Implement a comprehensive fall prevention plan during recovery. This includes home modifications, proper use of assistive devices, appropriate footwear, and balance exercises. Preventing falls during recovery is critical to avoid reinjury or additional injuries.
2. Protein Intake Optimization
Increase protein intake to support tissue repair, aiming for 1.2-1.5g/kg of body weight daily. Seniors often have increased protein requirements but decreased appetite, so focus on high-quality, easily digestible protein sources spread throughout the day.
3. Aquatic Therapy
Utilize water-based exercises when possible, as they reduce weight-bearing stress while providing resistance. Aquatic therapy is particularly beneficial for seniors as it allows for earlier movement with reduced pain and joint stress while maintaining muscle activation.
Universal Recovery Tips for All Age Groups
- Follow the RICE protocol (Rest, Ice, Compression, Elevation) during the acute phase
- Maintain consistent communication with your healthcare team
- Use appropriate bracing as directed by your physician
- Progress activities gradually based on pain and swelling response
- Stay hydrated and maintain balanced nutrition
- Avoid smoking and limit alcohol consumption
- Perform prescribed exercises with proper form rather than rushing through them
Medical Research on Age-Related MCL Healing

Research continues to enhance our understanding of age-related differences in ligament healing
Several key studies have investigated how age affects ligament healing, providing valuable insights into the biological mechanisms behind age-related recovery differences:
“Our findings demonstrate a clear correlation between patient age and MCL healing rates, with a progressive decline in healing capacity observed across the lifespan. Patients over 65 demonstrated approximately 40% longer healing times compared to adolescent patients with equivalent grade injuries.”
Key Research Findings
Cellular and Molecular Changes
A 2020 study in the American Journal of Sports Medicine found that fibroblast activity (cells responsible for collagen production) decreases by approximately 1-2% per year after age 30. The study demonstrated that tissue samples from older patients showed significantly reduced fibroblast proliferation and migration compared to younger patients, directly impacting the body’s ability to synthesize new collagen for ligament repair.
Vascular Response Differences
Research published in the Journal of Athletic Training (2018) used Doppler ultrasound to measure blood flow to healing MCL injuries across age groups. The study found that neovascularization (formation of new blood vessels) was 35% more robust in patients under 25 compared to those over 60, correlating with faster resolution of symptoms and return to function in younger patients.
Growth Factor Expression
A 2021 study in the Journal of Orthopaedic Research analyzed growth factor expression in healing MCL tissue. Researchers found that transforming growth factor-beta (TGF-β) and insulin-like growth factor-1 (IGF-1), both critical for ligament healing, showed significantly reduced expression in older subjects, with levels in seniors approximately 50-60% lower than in adolescents.
Collagen Quality Assessment
Biomechanical testing of healed MCL tissue (Clinical Orthopaedics and Related Research, 2019) revealed that not only does healing take longer in older individuals, but the resulting tissue has different properties. Healed ligaments in patients over 60 demonstrated 30% less tensile strength and decreased elasticity compared to similarly healed ligaments in patients under 30.
Clinical Application of Research
These research findings have important implications for clinical practice:
- Individualized timelines: Recovery protocols should be adjusted based on patient age rather than using standard timelines for all patients.
- Biological augmentation: Older patients may benefit from interventions that enhance the biological healing environment, such as platelet-rich plasma (PRP) injections, though more research is needed.
- Extended protection: Older patients likely benefit from longer periods of bracing and activity modification to accommodate slower healing rates.
- Nutritional support: Research suggests that targeted nutritional interventions may help compensate for age-related declines in healing capacity.
Common Myths About Age and MCL Recovery
Separating fact from fiction regarding age and MCL recovery
Myth #1: “If you’re over 40, you’ll never fully recover from an MCL tear.”
Fact: While healing does take longer with age, complete recovery is possible for patients of all ages with proper treatment. Studies show that over 90% of patients across all age groups can achieve functional recovery from MCL injuries, though the timeline and final outcome may vary. Older patients may need more time and specialized approaches, but age alone does not prevent full recovery.
Myth #2: “Younger patients don’t need to follow strict recovery protocols because they heal quickly anyway.”
Fact: While younger patients do heal faster, proper rehabilitation is still essential to ensure optimal outcomes. Adolescents and young adults who rush recovery or skip rehabilitation phases are at higher risk for reinjury and long-term instability. In fact, their active lifestyles may place greater demands on the healing ligament, making proper rehabilitation equally important despite faster biological healing.
Myth #3: “Surgery is always needed for MCL tears in older adults because they can’t heal naturally.”
Fact: Most MCL injuries, regardless of patient age, do not require surgery. Conservative treatment remains the standard of care for isolated MCL tears across all age groups. While healing takes longer in older adults, the MCL still has good healing potential due to its excellent blood supply. Surgery is typically reserved for complex tears or cases with multiple ligament involvement, not based on age alone.
Myth #4: “Anti-inflammatory medications speed up healing and should be used liberally.”
Fact: While NSAIDs can help manage pain and swelling, prolonged use may actually impair ligament healing. Research suggests that the inflammatory phase is a necessary part of the healing process. Current recommendations suggest limited use of anti-inflammatories during the acute phase (first 48-72 hours), particularly in older adults who already have reduced healing capacity.
Myth #5: “Once you reach a certain age, it’s not worth doing physical therapy for MCL injuries.”
Fact: Physical therapy remains essential for optimal recovery at any age. In fact, older adults often benefit more from structured rehabilitation than younger patients, as it helps address age-related deficits in strength, balance, and proprioception that could otherwise lead to chronic instability or reinjury. Modified, age-appropriate physical therapy protocols show excellent outcomes in senior populations.
Conclusion: Optimizing Your MCL Recovery Regardless of Age
Age significantly impacts MCL sprain healing time through biological mechanisms including reduced collagen production, decreased blood flow, and changes in cellular regeneration capacity. While younger patients generally heal faster, patients of all ages can achieve good functional outcomes with appropriate, age-specific treatment approaches.
The key to successful recovery lies in understanding these age-related differences and adapting treatment accordingly. Younger patients benefit from protocols that harness their robust healing capacity while preventing premature return to activities, while older adults require more comprehensive approaches that address longer healing timeframes and potential comorbidities.
By following age-appropriate rehabilitation guidelines, maintaining open communication with your healthcare team, and having realistic expectations based on your age group, you can optimize your recovery from an MCL sprain and return to your desired activities safely and effectively.
Get Expert Assessment for Your MCL Injury
Our sports medicine specialists can evaluate your specific MCL injury and create a personalized recovery plan based on your age, activity goals, and injury severity.
