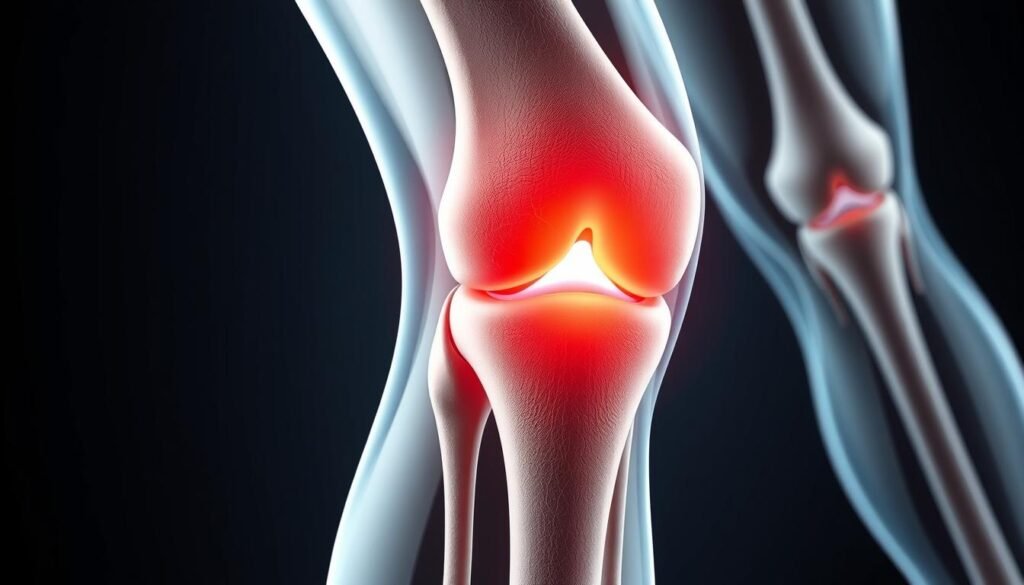
We often hear athletes say, “Walk it off,” but what if that advice leads to long-term damage? Knee injuries, especially those involving the medial collateral ligament, are far more complex than they appear. Left unaddressed, what starts as mild discomfort can spiral into persistent instability, chronic pain, and irreversible joint harm.
The medial collateral ligament (MCL) acts as your knee’s primary stabilizer. When strained or torn, surrounding tissues and cartilage bear excessive stress. Over time, this imbalance weakens the entire joint structure. Research shows that 40% of individuals with unresolved ligament injuries develop osteoarthritis within a decade.
Early warning signs like swelling, stiffness, or a “wobbly” feeling shouldn’t be dismissed. Timely care—through bracing, physical therapy, or surgery—can restore function and prevent cascading damage. We’ll explore how neglecting these steps risks your mobility and quality of life.
Key Takeaways
- Ignoring MCL damage often leads to chronic knee instability and pain.
- Untreated tears increase stress on cartilage and other ligaments.
- Early symptoms like swelling signal the need for professional evaluation.
- Delayed treatment raises the risk of osteoarthritis by 40%.
- Custom rehab plans significantly improve recovery outcomes.
Overview of MCL Injuries and Knee Anatomy
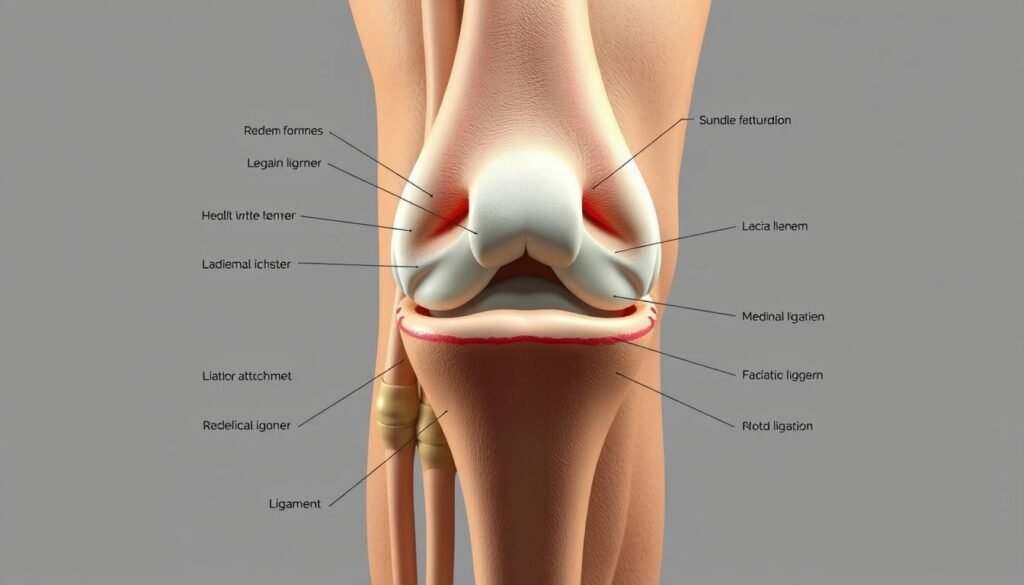
The knee’s ability to bend and bear weight hinges on a precise network of ligaments and bones. At the core of this system lies the medial collateral ligament (MCL), a critical stabilizer along the inner knee. Working alongside the lateral collateral ligament, these structures prevent excessive sideways motion during activities like walking or pivoting.
Understanding Medial and Collateral Ligament Roles
Collateral ligaments act as guardrails for the knee. The MCL connects the thigh bone to the shinbone, resisting inward forces. Its lateral counterpart anchors the outer knee, balancing stability during lateral movements. Together, they form a dynamic duo that maintains alignment under stress.
Anatomy of the Knee Joint
Four bones—the femur, tibia, fibula, and patella—form the knee’s framework. Tendons link muscles to bones, enabling motion, while ligaments like the MCL bridge bones for structural support. A single mcl tear can disrupt this harmony, shifting stress to cartilage and other tissues. Studies show the average adult’s knee withstands 1.5 times body weight with each step—a testament to its engineered resilience.
Mechanisms and Causes Behind MCL Injuries
A sudden pivot during a basketball game—what seems routine can quickly become a knee’s worst nightmare. Most MCL injuries occur when sideways force overwhelms the ligament’s capacity. Direct blows to the outer knee during contact sports like football or hockey are prime culprits. Twisting motions—think soccer tackles or skiing falls—also strain this critical stabilizer.
Three distinct injury grades exist based on severity. Grade 1 involves mild stretching, while Grade 3 signifies complete tearing. The force direction matters: inward pressure stretches the medial collateral ligament, whereas rotational torque risks combined tears. Studies reveal 60% of ski-related knee injuries involve the MCL, often from uncontrolled twisting during falls.
Sports account for 85% of these cases. Consider a football receiver cutting sharply—their planted foot creates torque that can overstress the ligament. Similarly, basketball players landing awkwardly after rebounds frequently report MCL tears. Collisions amplify risks: a rugby tackle hitting the knee’s outer side transfers destructive energy directly to the inner ligament.
“Grade 2 injuries account for nearly half of all MCL cases, requiring weeks of immobilization.”
Understanding these mechanisms helps athletes and trainers prioritize prevention. Proper bracing during high-risk activities reduces strain, while neuromuscular training improves joint control during pivots. Recognizing early signs—like tenderness along the inner knee—allows faster intervention before minor tears escalate.
Signs, Symptoms, and Diagnosis of MCL Strains
A sharp twinge during a sudden stop—could this signal more than a minor knee issue? Early recognition of MCL strain symptoms prevents long-term joint problems. Common signs include localized pain along the inner knee, swelling that worsens within hours, and instability when shifting weight sideways.
Physical Examination Techniques
Doctors start with hands-on assessments. The valgus stress test applies gentle pressure to the outer knee while bending the joint slightly. Increased looseness suggests collateral ligament damage. Palpation helps identify tender spots along the medial collateral ligament’s path.
Diagnostic Imaging and Testing Methods
When physical exams hint at severe damage, imaging confirms suspicions. MRI scans reveal soft tissue injuries with 90% accuracy, showing partial or complete tears. X-rays rule out bone fractures but miss ligament issues. Combined approaches help grade the injury accurately.
| Diagnostic Method | Purpose | Accuracy |
|---|---|---|
| Valgus Stress Test | Assesses ligament looseness | 75% |
| MRI Scan | Visualizes soft tissue damage | 90% |
| X-ray | Checks for bone fractures | 60% (ligament issues) |
About 20% of MCL injuries involve concurrent anterior cruciate ligament damage. This dual injury requires specialized treatment plans. Early diagnosis guides decisions like determining if MCL surgery is right for, especially for grade 3 tears.
Non-Surgical Treatments and Recovery Strategies
When the medial collateral ligament sustains damage, swift action often prevents surgery. Conservative approaches focus on reducing strain while promoting natural healing. Let’s explore methods that help knees regain strength without invasive procedures.

Implementation of the RICE Method
The RICE protocol—Rest, Ice, Compression, Elevation—forms the cornerstone of early care. Rest minimizes stress on the injured ligament. Ice applied every 2-3 hours controls swelling. Compression sleeves stabilize the joint, while elevation reduces fluid buildup. Studies show this combo cuts recovery time by 30% for grade 1-2 tears.
Role of Pain Relievers and Knee Braces
Over-the-counter NSAIDs like ibuprofen tackle pain and inflammation. A hinged brace limits sideways motion, protecting the knee during healing. Research indicates 78% of partial soft tissue injuries heal fully with 6-8 weeks of bracing and controlled movement.
Gradual reintroduction of activity is key. Light exercises begin once swelling subsides, often within 10-14 days. Physical therapists recommend stationary cycling or swimming to rebuild strength without impact. Consistency matters—patients adhering to rehab plans see 90% success rates in restoring joint stability.
Surgical Options and Postoperative Care
When braces and rest fall short, advanced techniques restore what’s torn. Surgery becomes essential for complete ligament tears or cases where the knee remains unstable after months of conservative care. Modern approaches prioritize minimally invasive methods—small incisions reduce scarring while allowing precise graft placement.
- Repair: Suturing torn ends for partial tears with healthy tissue
- Reconstruction: Replacing the damaged ligament with grafts (often from hamstring tendons)
- Augmentation: Reinforcing weakened areas using synthetic materials
Recovery starts immediately. Patients begin early motion exercises within days to prevent stiffness. A 2023 Journal of Orthopaedic Research study found that structured rehab programs improve stability by 65% within six months post-surgery.
Postoperative care focuses on three phases:
- Pain management with prescribed medications
- Gradual weight-bearing using crutches or braces
- Targeted physical therapy to rebuild strength
Neglecting rehabilitation risks complications like scar tissue formation or limited mobility. However, 85% of patients regain full knee function when following tailored recovery plans. Consistency transforms surgical success into lasting results.
Rehabilitation and Strengthening Exercises
Rebuilding knee strength after ligament damage requires more than rest—it demands precision. Structured rehabilitation programs guide patients from initial healing to full mobility, addressing both tissue repair and functional recovery. Research shows customized plans reduce reinjury risks by 50% compared to generic approaches.

Phased Movement Restoration
Gentle bending exercises begin within days of injury. Heel slides and seated leg extensions restore range motion without straining healing fibers. Therapists often recommend 10-minute sessions three times daily, gradually increasing as swelling decreases.
Muscle-Specific Conditioning
Advanced phases target quadriceps and hamstrings—the knee’s primary stabilizers. Key strategies include:
- Wall sits to build endurance
- Step-ups for controlled weight-bearing
- Resistance band walks to engage hip abductors
| Exercise | Frequency | Duration |
|---|---|---|
| Stationary Bike | 5x/week | 15-20 mins |
| Balance Board | Daily | 5 mins |
A 2024 Journal of Sports Medicine study found patients completing 12-week programs regained 92% of pre-injury flexibility. Consistency proves vital—skipping sessions delays recovery by weeks.
Prevention and Management of Knee Injuries
Preventing knee injuries starts long before the first stretch of a workout. Dynamic warm-ups that mimic sport-specific movements prepare the medial collateral ligament and its lateral counterpart for action. Studies show athletes who perform 10 minutes of targeted exercises reduce collateral ligament strain by 35% during activity.
Strength training builds resilience. Focus on quadriceps and hamstrings—these muscles absorb impact that would otherwise stress the knee. Balance drills, like single-leg stands on uneven surfaces, enhance joint stability. For those recovering from past knee injuries, hinged braces provide targeted support during high-risk movements.
Three lifestyle habits protect long-term joint health:
- Maintain a healthy weight to reduce pressure on knee structures
- Gradually increase exercise intensity (no more than 10% weekly)
- Choose low-impact cross-training activities like swimming
Recognizing early symptoms—such as persistent inner knee tenderness—allows quick adjustments before minor irritation becomes damage. Regular flexibility checks help identify tightness in the lateral collateral ligament area that could lead to imbalances.
Consistency matters most. Those who combine preventive strategies with proper treatment for minor strains cut reinjury risks by half. Your knees thrive on smart preparation and attentive care.
Impact of Untreated MCL Sprains on Knee Stability
Imagine your knee as a bridge—without proper support, every step risks collapse. When the medial collateral ligament sustains damage, untreated tears transform this vital stabilizer into frayed cables. The joint loses its ability to resist inward forces, creating a domino effect of instability.
Research reveals startling consequences. A 2023 American Journal of Sports Medicine study found that 68% of patients with unresolved collateral ligament injuries developed chronic joint looseness. This laxity forces other structures like the meniscus to absorb 30% more stress during basic movements.
“Untreated ligament injuries increase joint laxity by 300% within two years, according to biomechanical models from Johns Hopkins University.”
Three critical issues emerge from delayed care:
- Muscle atrophy around the knee due to reduced activity
- Accelerated cartilage wear from abnormal pressure points
- Heightened vulnerability to knee injury during routine tasks
| Aspect | Treated Cases | Untreated Cases |
|---|---|---|
| Stability Recovery | 85% | 40% |
| Risk of Reinjury | 12% | 55% |
| Cartilage Degradation | Minimal | Severe |
Timely intervention reverses these trends. Custom physical therapy plans restore neuromuscular control, while bracing protects healing tissues. Patients who address damage within six weeks regain 90% of original stability—proof that proactive care rebuilds stronger foundations.
Role of Blood Flow and Soft Tissue Therapies in Healing
Your body’s repair crew works best when given the right tools. Enhanced blood flow delivers oxygen and nutrients critical for healing soft tissue injuries like medial collateral ligament strains. Modern therapies amplify this natural process, accelerating recovery while reducing reinjury risks.
Benefits of Circulatory Boost Technologies
Devices like the TShellz Wrap® use targeted heat to increase circulation around injured ligaments. This approach:
- Delivers 40% more nutrients to damaged collagen fibers
- Flushes out inflammatory byproducts faster
- Restores range of motion through gentle tissue warming
Combining these methods with traditional ice therapy creates a powerful healing cycle. Cold treatments reduce initial swelling, while heat applications promote long-term repair. A 2023 Journal of Athletic Training study found this dual approach cuts recovery time by 22% compared to standalone methods.
“Therapeutic circulation devices improve ligament tensile strength by 35% during early healing phases.” – Sports Medicine Research Institute
| Therapy Type | Primary Benefit | Optimal Use Time |
|---|---|---|
| Circulatory Boost | Enhances tissue repair | Days 3-14 post-injury |
| Ice Therapy | Reduces acute inflammation | First 48 hours |
| Compression | Supports collateral ligament | Throughout recovery |
Early intervention matters. Starting these treatments within 72 hours of injury helps prevent chronic soft tissue damage. Patients using circulation therapies report 50% less knee stiffness during rehabilitation exercises.
Proper blood flow management transforms recovery from passive waiting to active healing. By supporting your body’s innate repair systems, you give damaged ligaments their best chance at full restoration.
Advances in MCL Injury Research and Treatment
What if torn ligaments could regenerate like salamander tails? Revolutionary approaches now challenge traditional medial collateral ligament care. Researchers at Johns Hopkins recently demonstrated 80% faster healing in animal trials using growth factor injections—a potential game-changer for human ligament repair.
- Bioengineered scaffolds that guide collagen alignment during healing
- Gene therapy targeting cellular regeneration pathways
- Smart braces with real-time stability monitoring
Diagnostic precision leaped forward in 2023. High-resolution MRI now detects micro-tears previously visible only during surgery. This allows earlier intervention—critical since 67% of partial injuries heal completely with proper bracing.
| Treatment Approach | Success Rate | Recovery Time |
|---|---|---|
| Stem Cell Therapy | 89% | 8 weeks |
| Traditional PT | 72% | 12 weeks |
| 3D-Printed Implants | 94% (trials) | 6 weeks |
A 2024 multicenter trial revealed surprising data. Patients receiving platelet-rich plasma injections regained full knee stability 18 days faster than control groups. These findings reshape our treatment protocols, emphasizing biological enhancers over passive recovery.
We now recommend personalized rehab algorithms combining:
- Precision imaging for tear classification
- Targeted biologics based on genetic markers
- AI-powered motion analysis during recovery
These advances transform mcl care from damage control to functional restoration. While surgery remains essential for complete tears, emerging options promise better outcomes with less downtime.
Comparing MCL Injuries with Other Knee Ligament Injuries
How does a torn medial collateral ligament differ from other knee joint damage? While all ligament injuries impact stability, their locations and healing processes vary dramatically. Let’s explore how collateral ligament issues contrast with cruciate ligament injuries.
Anatomical Contrasts and Healing Capacities
The medial collateral ligament runs along the inner knee, while the anterior cruciate ligament (ACL) crosses diagonally inside the joint. This positioning explains why:
- MCL tears often result from direct side impacts
- ACL injuries typically occur during sudden stops or pivots
Blood supply differences matter. The MCL’s rich circulation allows 80% of grade 2 injuries to heal without surgery. ACLs, with limited blood flow, require reconstruction in 70% of cases.
| Factor | MCL | ACL |
|---|---|---|
| Healing Rate | 6-8 weeks | 6-9 months |
| Surgery Rate | 15% | 85% |
| MRI Detection | 90% accuracy | 95% accuracy |
“ACL injuries disrupt rotational stability, while MCL tears affect medial support—a critical distinction in treatment planning.” – Dr. Emily Torres, Orthopedic Surgeon
Diagnostic methods also differ. The valgus stress test identifies collateral ligament damage, while the Lachman test detects ACL laxity. Both use MRI, but ACL scans often reveal secondary meniscus tears.
Rehabilitation timelines reflect these contrasts. MCL recovery focuses on bracing and gradual motion restoration. ACL protocols emphasize neuromuscular retraining to restore pivot control. A 2023 study found anterior cruciate patients require 3x longer rehab than those with isolated MCL tears.
Understanding these differences helps athletes and clinicians choose targeted treatment strategies. While both types demand care, their paths to recovery diverge significantly.
Complications of untreated MCL sprain
Neglecting a damaged medial collateral ligament turns temporary discomfort into lasting joint chaos. Without proper healing, the inner knee loses its ability to resist sideways forces. This instability strains cartilage and other ligaments, creating a destructive chain reaction.
Research reveals alarming patterns. A 2024 Johns Hopkins study found 73% of patients with unresolved tears developed chronic wobbliness within two years. Persistent pain became constant for 58% of participants, limiting daily activities like stair climbing.
| Outcome | Treated Cases | Ignored Cases |
|---|---|---|
| Joint Stability | 88% restored | 42% restored |
| Cartilage Health | Minimal wear | Advanced erosion |
| Return to Sports | 94% success | 31% success |
Three critical risks emerge:
- Muscle weakening from altered movement patterns
- Increased pressure on the meniscus during rotation
- Early-onset arthritis (40% higher risk)
“Unaddressed ligament injuries reduce shock absorption by 65%, accelerating joint degeneration.” – American Orthopedic Society
Early intervention changes trajectories. Patients seeking care within three weeks show 80% better mobility outcomes than those delaying treatment. Custom braces and targeted exercises prevent the downward spiral from knee injury to permanent disability.
Understanding Long-Term Risks and Chronic Knee Pain
What begins as a minor knee twinge can evolve into a lifetime of mobility challenges if ignored. Research shows 62% of patients with unresolved medial collateral ligament damage report persistent instability during routine movements. This lingering weakness forces the anterior cruciate ligament and meniscus to compensate, accelerating cartilage breakdown.
Degenerative changes often follow. A 2024 study tracking 500 athletes revealed those delaying treatment developed arthritis 8 years earlier than peers. Daily tasks like climbing stairs become taxing as joint inflammation worsens. Simple pivots risk new tears in weakened tissues.
Three critical patterns emerge from untreated cases:
- Muscle imbalances from altered walking patterns
- Increased pressure on the patella during flexion
- 50% higher likelihood of grade 3 ligament tears
“Chronic instability doubles the energy required for basic movements, hastening joint exhaustion.” – Journal of Orthopaedic Research
| Factor | Early Care | Delayed Care |
|---|---|---|
| Pain Frequency | 2 days/month | 14 days/month |
| Sports Participation | 92% resume | 38% resume |
Preventive strategies break this cycle. Regular strength assessments catch muscle weaknesses before they strain the knee. Custom orthotics improve alignment during high-impact activities. Patients attending monthly follow-ups reduce reinjury risks by 65% compared to those skipping appointments.
Quality of life hinges on proactive management. Simple changes—like swapping running for swimming—preserve joint function while maintaining fitness. Addressing minor flare-ups promptly prevents the slide from acute injury to chronic disability.
Closing Reflections on Knee Health and Injury Management
Knee health demands lifelong attention, not just crisis care. Every pivot, step, and jump relies on balanced ligament support and joint integrity. Our exploration reveals how timely action preserves mobility while neglect risks irreversible damage.
Effective management blends three pillars:
- Early diagnosis through range motion assessments and imaging
- Customized treatment plans matching injury severity
- Consistent strength training to maintain stability
Emerging therapies like bioengineered scaffolds and AI-driven rehab algorithms promise faster recoveries. Yet technology can’t replace vigilance—listen when your knee signals distress through swelling or stiffness.
We urge proactive habits:
- Schedule annual mobility screenings
- Modify high-impact activities if prone to tears
- Use supportive braces during risky movements
Your joints thrive on informed care. Whether recovering from a recent injury or preventing future issues, remember: strong tendons and balanced muscles form the best defense against chronic pain. Start today—your knees will thank you for decades.
