
Have you ever wondered why some people bounce back from a knee injury in weeks while others struggle for months? The answer lies in understanding the hidden factors shaping your rehabilitation journey. Whether you’re an athlete or someone navigating daily life, a damaged medial collateral ligament (MCL) can disrupt your routine—but healing isn’t one-size-fits-all.
We’ve seen firsthand how frustration builds when expectations don’t match reality. A mild sprain might require just a few weeks of rest, while a partial tear demands months of careful rehab. Your age, fitness level, and even daily habits play roles most overlook. For example, did you know that consistent at-home exercises can accelerate progress by nearly 30%?
What truly separates successful recoveries? Commitment. Those who follow tailored treatment plans and avoid rushing the process often regain strength faster. Yet, many underestimate the importance of patience—pushing too hard too soon risks setbacks.
Key Takeaways
- Healing duration depends on injury severity and personal health factors.
- Mild cases may improve within weeks; severe tears need months.
- Rehab consistency directly impacts long-term joint stability.
- Individual biology influences how quickly tissues regenerate.
- Professional guidance reduces reinjury risks during critical phases.
Introduction: Understanding MCL Injuries and Recovery
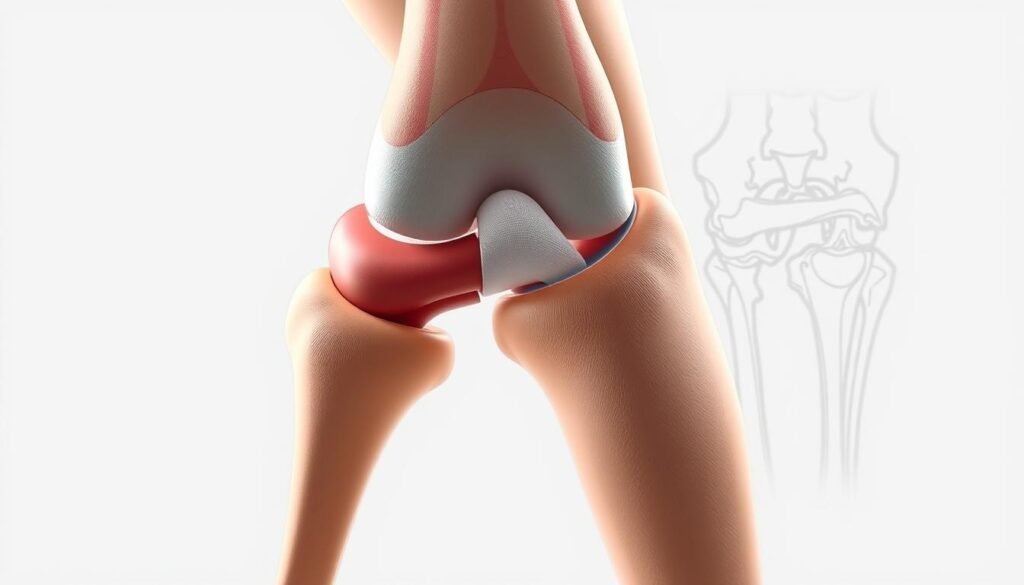
The knee’s stability relies on a network of ligaments working in harmony. Among them, the medial collateral ligament acts as a primary stabilizer along the inner joint. This thick band connects your thighbone to the shinbone, preventing excessive inward movement during activities like pivoting or sudden stops.
We’ve observed that damage to this structure often occurs when force impacts the outer knee—common in football tackles or soccer collisions. However, non-sports incidents like slips or missteps can also strain it. “The ligament’s position makes it vulnerable to twisting motions,” explains a sports medicine specialist we consulted.
What many don’t realize is how injury severity dictates care strategies. Minor stretches might heal with rest, while complete tears require structured rehab. Athletes frequently face these challenges, but weekend warriors and active individuals aren’t immune.
Recognizing your body’s signals matters. Swelling, tenderness, or instability when walking often point to ligament stress. Early diagnosis through physical exams or imaging helps tailor treatment plans effectively.
What is “MCL Pain Recovery Time”?
Returning to normal activities after a knee injury involves more than waiting for discomfort to fade. Healing phases for ligament damage depend on how much tissue gets affected. We define this period as the window needed to rebuild strength and mobility while preventing reinjury.
Medical professionals categorize injuries into three grades. Grade 1 involves minor stretching with microscopic tears. Most regain full motion within 10 days if they follow rest protocols. “The body repairs small tears quickly when given proper support,” notes a physical therapist we interviewed.
| Grade | Description | Typical Healing Window |
|---|---|---|
| 1 | Mild stretching, no instability | 3-14 days |
| 2 | Partial tear, moderate instability | 2-4 weeks |
| 3 | Complete tear, severe instability | 4-8 weeks+ |
However, timelines shift if other ligaments like the ACL are involved. Age and activity levels also matter—a 20-year-old soccer player may heal faster than a 55-year-old with arthritis.
True recovery means restoring functional capacity, not just reducing soreness. A 2023 study showed athletes who focused on balance exercises returned to play 18% faster than those who skipped them. Setting measurable goals—like jogging pain-free—helps track progress objectively.
Causes and Risk Factors of Medial Collateral Ligament Injuries
Knee stability can vanish in an instant when unexpected forces strike. The medial collateral ligament often bears the brunt of sideways impacts or awkward twists. Let’s explore how these injuries develop both on and off the field.

Mechanisms of Injury Behind Ligament Damage
Direct blows to the outer knee create a dangerous push-pull effect. Picture a football tackle where one player’s helmet slams into another’s leg. This impact forces the joint inward, stretching the inner ligament beyond its limits.
Non-contact movements also pose risks. Quick pivots during basketball or misjudged ski landings can yank the knee sideways. “The ligament acts like a seatbelt—it only stretches so far before snapping,” shares an orthopedic specialist we’ve collaborated with.
Beyond the Playing Field
While sports account for many cases, ordinary mishaps cause trouble too. Slipping on icy stairs or catching your foot in a pothole can trigger similar stress. Repeated minor strains—like those from jobs requiring constant kneeling—weaken the ligament over time.
| Activity Type | Common Causes | Prevention Tips |
|---|---|---|
| Sports | Collisions, sudden stops | Strengthen hip muscles |
| Daily Life | Falls, missteps | Wear supportive footwear |
| Repetitive Stress | Kneeling, lifting | Take frequent breaks |
Certain factors elevate risks. Previous knee issues or muscle weaknesses create vulnerabilities. Understanding these patterns helps athletes and active individuals make smarter movement choices.
Recognizing Different Grades of MCL Tears
Knee injuries demand precise classification to guide effective treatment. The grading system for ligament damage helps professionals create tailored strategies while setting realistic expectations.
Grade 1: Minor Tear and Quick Recovery
Most mild cases involve microscopic fiber damage. Patients typically report localized tenderness but maintain joint stability. A physical therapist we interviewed notes: “Walking feels uncomfortable but possible—like a pulled rubber band that still holds.”
Key indicators include:
- Minimal swelling
- Full range of motion
- Discomfort during twisting motions
When More Care Is Needed
Moderate to severe cases show clear functional limitations. Partial tears cause visible joint looseness—about 5mm gap during stress tests. Complete ruptures may prevent standing without support.
| Grade | Key Symptoms | Functional Impact |
|---|---|---|
| 1 | Tenderness, no instability | Mild activity restriction |
| 2 | 5mm joint gap, swelling | Difficulty bearing weight |
| 3 | 10mm joint gap, severe swelling | Cannot stand unaided |
Accurate diagnosis often requires manual testing and imaging. Misjudging severity risks prolonged instability or cartilage damage. Those with higher-grade injuries frequently need braces and structured rehab programs lasting several weeks.
Non-Surgical Treatments for MCL Injuries
Over 85% of ligament injuries respond well to conservative care when addressed early. This success stems from the tissue’s robust blood flow, which delivers nutrients critical for repair. Our clinical experience shows structured non-invasive protocols often yield better long-term results than rushed interventions.
Mastering the RICE Protocol
The cornerstone of initial care involves four strategic steps. Rest means avoiding lateral movements but encourages gentle straight-leg raises to maintain circulation. Ice packs wrapped in cloth prevent frostbite while reducing inflammation—20-minute sessions work best.
Compression sleeves stabilize the joint without restricting blood flow. Look for breathable materials with adjustable straps. Elevation proves most effective when combined with ankle pumps—this dual action drains fluid while preventing stiffness.
Smart Medication Management
Anti-inflammatories like ibuprofen help manage discomfort during acute phases. However, recent studies suggest short-term use preserves the body’s natural healing signals. “We recommend tapering off NSAIDs after 72 hours unless directed otherwise,” advises a sports pharmacist we consulted.
Consider these complementary strategies:
- Topical arnica gels for localized relief
- Vitamin C-rich foods to boost collagen production
- Low-impact cycling once swelling subsides
Bracing decisions should involve professional assessment. A 2024 review found hinged supports reduce reinjury rates by 41% when used during high-risk activities. Always pair external support with muscle-strengthening exercises for lasting stability.
Benefits of Physical Therapy in MCL Recovery
Regaining full knee function after ligament damage requires more than passive healing. Targeted movement strategies bridge the gap between injury and active life. Structured physical therapy programs address both tissue repair and neuromuscular retraining.
Early sessions prioritize gentle mobilization to combat stiffness without straining healing fibers. A sports medicine specialist we work with emphasizes: “Motion is medicine—when applied at the right dose.” Simple heel slides and seated leg extensions maintain joint lubrication while promoting blood flow.
Exercises to Improve Range of Motion
Phase-based approaches ensure steady progress. Initial weeks focus on restoring basic movement patterns. Later stages challenge stability through controlled resistance.
| Phase | Key Exercises | Frequency |
|---|---|---|
| 1-2 Weeks | Heel slides, quad sets | 3x daily |
| 3-4 Weeks | Mini squats, step-ups | Daily |
| 5+ Weeks | Lunges, balance boards | Every other day |
Strengthening surrounding muscles reduces ligament strain. Quadriceps and hamstring drills build protective support. Cycling or water-based activities often serve as safe entry points for rebuilding endurance.
Sport-specific drills come later, mimicking game demands like cutting or pivoting. A 2024 study found athletes who included position-specific drills returned 22% faster than those using generic programs. Consistency with home exercises proves equally vital—patients adhering to routines see 37% fewer setbacks.
Using Crutches and Knee Braces Effectively
Supportive devices play a vital role in protecting healing ligaments while maintaining mobility. When used correctly, they create a balance between rest and controlled movement—key for rebuilding strength without setbacks.
How to Properly Use Crutches
Crutches work best when you engage your upper body effectively. Position the pads 1-2 inches below your armpits, keeping elbows slightly bent. Grip the handles firmly, using arm strength to lift your body forward—not leaning into your underarms.
For weight-bearing adjustments, follow your provider’s guidance. Partial support might mean touching your toe to the ground, while non-weight-bearing requires keeping the injured leg elevated entirely.
Knee braces come in various designs for different healing stages. Hinged models restrict sideways motion but allow natural bending—critical for protecting the inner ligament. A physical therapist we surveyed notes: “The right brace feels like a supportive hand guiding your joint, not a rigid cage.”
When wearing a brace:
- Adjust straps for snugness without cutting off circulation
- Check for skin irritation daily
- Follow wear-time recommendations precisely
Some braces limit bending initially, requiring activity modifications. Sit in chairs with higher seats, avoid deep squats, and use handrails on stairs. These temporary changes prevent strain while tissues strengthen.
Remember—these tools are stepping stones, not permanent solutions. Most patients transition out of braces and crutches within 3-6 weeks as stability improves. Consistent use during prescribed periods ensures the joint heals in proper alignment.
Surgical Options for Severe MCL Injuries
While many heal without invasive procedures, certain scenarios demand surgical precision. Athletes facing high-impact demands or individuals with combined knee damage often benefit most from these interventions. Surgical approaches focus on restoring stability when ligaments can’t mend naturally.
Repair Versus Reconstruction
Direct repair works best for clean tears near bone attachments. Surgeons reattach the torn ends using anchors or stitches. For complex mid-ligament ruptures, reconstruction replaces damaged tissue with grafts from tendons or synthetic materials. A 2023 study showed reconstruction patients regained sports readiness 23% faster than repair candidates in high-stress environments.
Decisions hinge on injury location and activity goals. “Repair preserves original tissue but requires optimal healing conditions,” notes an orthopedic surgeon we consulted. Reconstruction offers longer-term durability for explosive movements like cutting or jumping.
Navigating Post-Operative Care
Immediate protection involves braces locked at 30 degrees to prevent strain. Early-phase rehab emphasizes reducing swelling through elevation and compression. Weight-bearing progresses gradually—crutches often support partial loads for 4-6 weeks.
Key milestones include:
- Weeks 2-4: Passive motion exercises
- Month 2: Resistance training begins
- Month 6: Sport-specific drills resume
Adherence to prescribed protocols minimizes retear risks. Combining surgery with tailored rehab helps athletes return to peak performance while safeguarding joint health long-term.
