
Have you ever wondered why some knee injuries linger despite weeks of limited activity? The medial collateral ligament (MCL) acts like a hidden anchor, keeping your joint stable during movements. When damaged, even simple tasks like walking or standing can feel impossible. But what truly determines recovery success?
This critical band of tissue prevents excessive side-to-side motion. Injuries range from mild stretches to complete tears, each demanding specific care strategies. While many assume time heals all, improper management often leads to chronic weakness or reinjury.
We’ll explore how modern approaches combine targeted therapies with personalized plans. From braces to progressive exercises, effective solutions exist beyond generic advice. Understanding your injury’s severity helps match interventions to your unique needs.
Key Takeaways
- The MCL stabilizes the knee during lateral movements
- Injury grades determine recovery timelines and methods
- Early intervention prevents long-term joint complications
- Combination therapies often yield better outcomes than single approaches
- Professional assessment ensures proper diagnosis and care alignment
Understanding MCL Pain Treatment and the Medial Collateral Ligament
Inside your knee lies a critical stabilizer that works silently during every step. This structure maintains balance when changing directions or absorbing impact. Let’s explore its anatomy and common injury patterns.
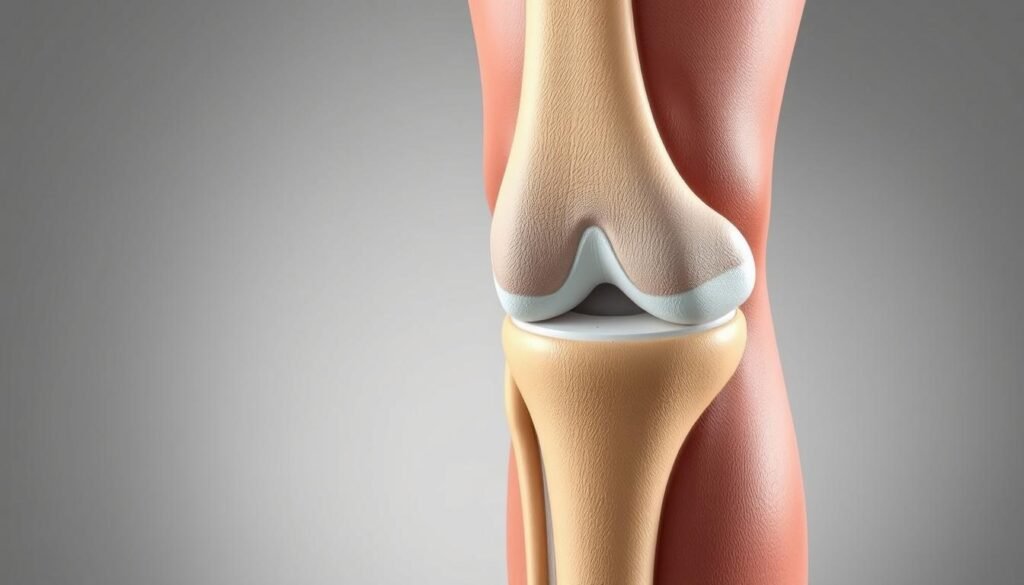
Anatomy of a Key Stabilizer
The medial collateral ligament stretches along your knee’s inner side, linking thighbone to shinbone. Its broad, flat design resists inward leg movements while permitting natural rotation. This dual function makes it essential for walking, running, and pivoting.
Three features define this ligament’s effectiveness:
- Thick collagen fibers withstand lateral forces
- Connective tissue merges with joint capsule for added support
- Strategic positioning 1-2 inches below the knee joint optimizes leverage
Mechanisms of Injury
Sudden impacts to the knee’s outer side often strain or tear this ligament. Athletes frequently experience this during tackles or awkward landings. Non-contact injuries occur when twisting the leg while the foot remains planted.
Common scenarios include:
- Football collisions forcing the knee inward
- Skiing falls with locked boots
- Missteps on uneven surfaces causing uncontrolled rotation
Causes and Risk Factors of MCL Injuries
What separates weekend warriors from professional athletes when it comes to knee damage? While intense physical activity plays a role, unexpected everyday motions can be equally hazardous. Let’s break down the primary culprits behind ligament strain.
Common Causes in Sports
High-impact activities account for 62% of reported cases according to sports medicine studies. Football remains a top offender due to lateral tackles that twist knees at unnatural angles. Soccer players face similar risks during sudden pivots, while basketball athletes often injure themselves during awkward landings.
“The force generated during a blindside tackle can exceed 800 Newtons – enough to compromise even healthy ligaments.”
Three sports with elevated risk:
- Rugby: Frequent collisions and scrums
- Martial arts: Dynamic kicks and takedowns
- Alpine skiing: Fixed boots increase torque during falls
Non-Athletic Injury Triggers
Accidental slips on wet floors cause 28% of non-sports related cases. Other scenarios include:
| Activity | Mechanism | Prevention Tip |
|---|---|---|
| Car accidents | Dashboard impact forces knee inward | Adjust seat position |
| Heavy lifting | Twisting while carrying weight | Use proper form |
| Frozen surfaces | Legs splaying outward | Wear traction aids |
Repetitive stress from occupations requiring kneeling or squatting gradually weakens ligament integrity. Construction workers and landscapers often develop chronic issues without proper ergonomics.
Recognizing Symptoms of MCL Tears
How does your body signal that something’s wrong after a knee twist? Early identification of ligament issues prevents long-term complications. Let’s break down the warning signs that demand attention.

Pain, Popping, and Tenderness
A sharp discomfort along the inner knee often marks the first clue. Many report hearing or feeling a distinct pop during sudden twists or impacts. This sound typically accompanies immediate tenderness when pressing the affected area.
Sensitivity levels vary widely. Some experience mild soreness when bending, while others struggle to put weight on the leg. Bruising may appear within hours, tracing the ligament’s path from thigh to shin.
Swelling and Knee Instability
Fluid buildup around the joint usually develops within 24 hours. The inner knee might feel warm or look puffy compared to the unaffected side. This inflammation often limits movement range and causes stiffness.
Functional challenges become apparent during daily activities. Patients frequently describe:
- A sensation of the leg “giving out” when shifting weight
- Difficulty straightening or fully bending the joint
- Persistent tightness despite rest
“Ignoring these signs risks further damage to surrounding tissues,” notes a sports medicine specialist. Prompt evaluation determines whether the ligament sustained partial or complete tearing.
Grading and Diagnosis of MCL Injuries
Medical professionals use precise classification systems to map recovery pathways. Accurate injury categorization guides everything from brace selection to rehabilitation timelines.
Understanding Injury Severity Levels
Grade 1 injuries involve stretched fibers without tearing. Patients typically maintain joint stability but report tenderness along the inner knee. Most resume light activities within 1-2 weeks.
Partial ruptures define Grade 2 tears. This mid-level damage creates noticeable looseness during side movements. Swelling often accompanies moderate pain, requiring 4-6 weeks of controlled motion therapy.
Complete ligament separation marks Grade 3 cases. The joint becomes unstable, with severe discomfort during weight-bearing. “These injuries frequently coincide with ACL damage,” notes orthopedic surgeon Dr. Elena Torres. “Comprehensive imaging prevents missed diagnoses.”
Advanced Diagnostic Approaches
Magnetic resonance imaging (MRI) delivers detailed soft tissue analysis. This technology identifies 90% of ligament abnormalities, distinguishing partial tears from full ruptures. Radiologists assess fiber alignment and swelling patterns.
X-rays rule out bone fractures, while ultrasound monitors healing progress. Three imaging factors determine exam choices:
- Symptom persistence beyond 72 hours
- Visible joint deformity
- Failed stability tests during physical exams
Clinicians often combine multiple techniques for complex cases. This layered approach ensures tailored treatment plans matching each injury’s unique characteristics.
Non-Surgical Treatment Options: Rest, Ice, and More
When ligaments sustain damage, the body’s innate healing abilities often make surgery unnecessary. Conservative approaches leverage natural recovery processes while protecting the joint from further stress. Over 80% of cases resolve successfully through structured protocols combining immediate care and progressive rehabilitation.
The RICE Method Explained
Rest prevents additional strain during the critical first 72 hours. Ice application every 2-3 hours reduces inflammation, while compression bandages stabilize the area. Elevation above heart level encourages fluid drainage, accelerating healing.
This approach works exceptionally well due to the ligament’s robust blood supply. Unlike other connective tissues, this vascular network delivers nutrients needed for repair. Most patients notice reduced swelling within five days when following RICE consistently.
Physical Therapy and Rehabilitation Exercises
Structured movement begins once acute symptoms subside. Therapists often start with gentle stretches to restore flexibility. A phased program might include:
- Seated leg raises to reactivate muscles
- Controlled bends to improve joint mobility
- Balance drills to rebuild stability
Progress to resistance training typically occurs around week three. “Consistency matters more than intensity during early phases,” advises physical therapist Marco Ruiz. Full recovery usually aligns with the six-week mark, though individual timelines vary based on injury grade and adherence to protocols.
When to Consider Surgery for MCL Pain Treatment
While most knee ligament injuries heal without surgery, certain scenarios demand precise medical intervention. We’ll clarify when operating becomes essential for restoring full mobility and preventing chronic instability.
Surgical Procedures and Techniques
Complete tears with joint instability often require reconstruction. Surgeons typically choose between two approaches:
- Direct repair: Reattaching torn ends using sutures or anchors
- Graft reconstruction: Replacing damaged tissue with tendons from the patient’s hamstring or a donor
“Modern arthroscopic methods reduce recovery time by 40% compared to open surgery,” notes Dr. Alicia Chen, orthopedic specialist.
| Procedure | Best For | Recovery Start |
|---|---|---|
| Direct Repair | Fresh tears with viable tissue | 2-3 weeks |
| Graft Reconstruction | Chronic injuries or multiple ligament damage | 6-8 weeks |
Post-Surgery Recovery and Management
Rehabilitation focuses on restoring strength without straining repairs. Patients typically:
- Use braces for 4-6 weeks to limit sideways motion
- Begin weight-bearing exercises by week 3
- Graduate to sport-specific drills after 12 weeks
Regular checkups track healing progress. Athletes often return to competition within 6-9 months, depending on graft integration and muscle retraining success.
Role of Physical Therapy in MCL Recovery
Rebuilding joint stability after injury requires more than rest—it demands strategic movement. Structured rehabilitation programs address both healing tissues and functional needs. Physical therapy bridges the gap between injury and full activity through science-backed methods.
Customized Exercise Regimens
Clinicians design programs around three factors: injury severity, daily demands, and recovery goals. Initial sessions focus on restoring gentle motion. Later phases introduce resistance training to fortify surrounding muscles.
“Our programs evolve as the ligament heals,” explains physical therapist Dr. Maya Singh. “Early phases protect the area, while later stages rebuild dynamic stability.”
Key components include:
- Quadriceps activation: Seated leg lifts prevent muscle atrophy
- Controlled cycling: Boosts circulation without joint stress
- Balance drills: Improve proprioception for injury prevention
Athletes receive sport-specific modules mimicking game movements. Soccer players might practice cutting drills, while runners focus on gait retraining. This tailored approach reduces re-injury risks by 34% compared to generic plans.
Consistency determines outcomes. Most patients achieve full mobility within 6-12 weeks when following prescribed exercises. Regular progress assessments ensure therapies align with healing timelines.
Using Braces and Crutches for Support
Optimal recovery strategies incorporate devices that restrict harmful movements while promoting healing. These tools protect vulnerable tissues during daily activities, allowing natural repair processes to work effectively. Medical professionals often recommend combining stabilization gear with mobility aids for balanced recovery.
Matching Support to Needs
Hinged braces with rigid side panels prevent inward knee motion, ideal for moderate MCL injuries. Adjustable straps customize compression, while breathable materials reduce skin irritation. Specialists assess gait patterns and swelling levels to select the right design.
Crutches help offload weight during early healing phases. Proper sizing ensures handles align with hip height, keeping elbows slightly bent. Rubber tips improve traction, and padded grips prevent hand fatigue during extended use.
Combining these tools creates a protective framework for tissue repair. Most users transition to partial weight-bearing within 14-21 days as strength returns. Regular adjustments maintain alignment with evolving recovery goals, reducing reinjury risks.
