
When someone experiences inner-leg joint discomfort, most assume it’s just a temporary strain. But what if that ache signals something deeper? Properly identifying the source requires careful evaluation, especially since symptoms often overlap across conditions.
In primary care, this challenge is common. A single symptom could stem from soft tissue damage, cartilage wear, or even referred issues from nearby areas. That’s why narrowing down possibilities demands both precision and expertise.
We’ll explore how subtle differences in location, movement patterns, and injury history shape the assessment process. By focusing on anatomical structures and functional relationships, clinicians can untangle complex cases more effectively.
Key Takeaways
- Inner-leg joint issues are among the most frequent patient complaints in clinics.
- Multiple factors contribute to symptoms, requiring systematic evaluation.
- Anatomy plays a pivotal role in distinguishing between similar conditions.
- Trauma and overuse injuries often present with overlapping characteristics.
- A stepwise diagnostic approach improves accuracy and treatment outcomes.
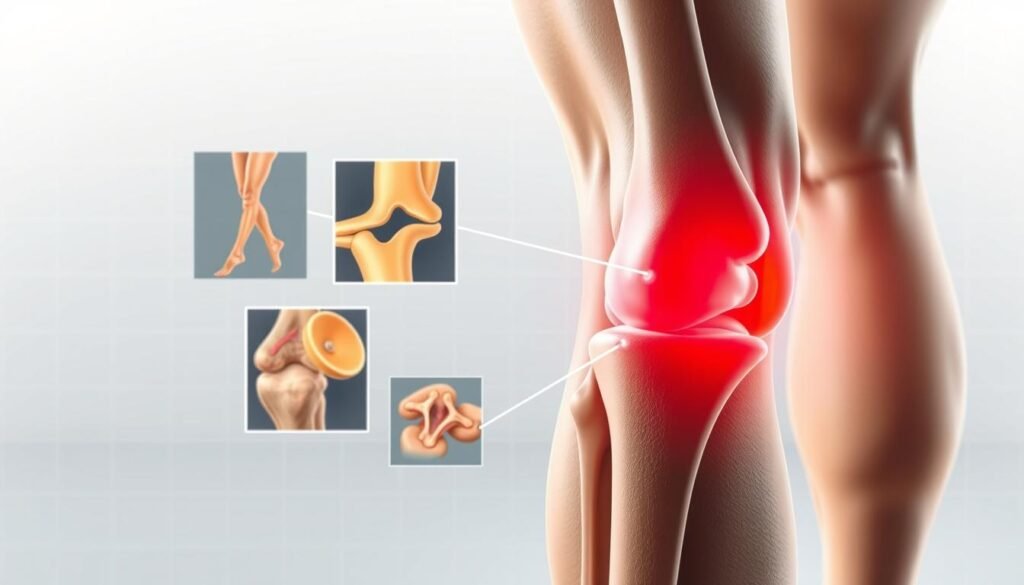
Understanding the Knee Anatomy and Medial Structures
Stability during movement isn’t accidental—it’s built through interconnected anatomical systems. The largest joint in the body functions like a precision machine, distributing forces across bones, cartilage, and soft tissues. At its core, the knee joint acts as a hinge, transferring weight from the hips to the ground while allowing controlled rotation.
Knee Joint Overview and Biomechanics
Three bones form this joint: the femur, tibia, and patella. Between them, the medial meniscus cushions impacts and reduces friction during walking or running. This crescent-shaped cartilage absorbs up to 50% of compressive loads, protecting bones from wear.
Key Medial Structures: Ligaments, Meniscus, and Bursa
The collateral ligament on the inner side prevents excessive sideways motion. Paired with the quadriceps muscles, it maintains alignment during sudden stops or pivots. Weakness here often leads to instability, emphasizing the ligament’s role in daily activities.
Biomechanical stress tests reveal how ligament integrity affects joint health. For example, repetitive twisting strains the medial meniscus, while weakened quadriceps shift pressure to surrounding tissues. Recognizing these relationships helps clinicians pinpoint vulnerabilities before symptoms escalate.
Causes and Injury Mechanisms Behind Medial Knee Pain
Understanding why discomfort arises requires exploring two distinct pathways: gradual wear and sudden damage. Both pathways strain the same anatomical structures but demand different diagnostic approaches.
Overuse Syndromes and Repetitive Stress Factors
Daily activities like running or climbing stairs can quietly erode joint health. A dull ache that worsens with movement often signals repetitive injury. Swelling might develop gradually, masking underlying damage to cartilage or tendons.
Common culprits include:
- Meniscus tear from repeated twisting motions
- IT band tightness redirecting stress to inner structures
- Bursa inflammation due to friction
Acute Trauma and Ligamentous Injuries
Sudden impacts change the game completely. A collision or awkward fall might rupture the collateral ligament – a traumatic event often accompanied by immediate swelling. Patients frequently report hearing a “pop” before sharp pain sets in.
Key indicators of severe trauma include:
- Inability to bear weight
- Visible joint deformity
- Rapid bruising around the affected area
Whether from chronic strain or abrupt force, proper evaluation prevents misdiagnosis. We prioritize identifying whether symptoms stem from cumulative stress or a single catastrophic event.
Medial knee pain differential diagnosis: Identifying Underlying Conditions
Not all inner-joint aches stem from the same source—some hide complex origins. We prioritize distinguishing subtle differences between pathologies that share similar symptoms but demand distinct treatments.
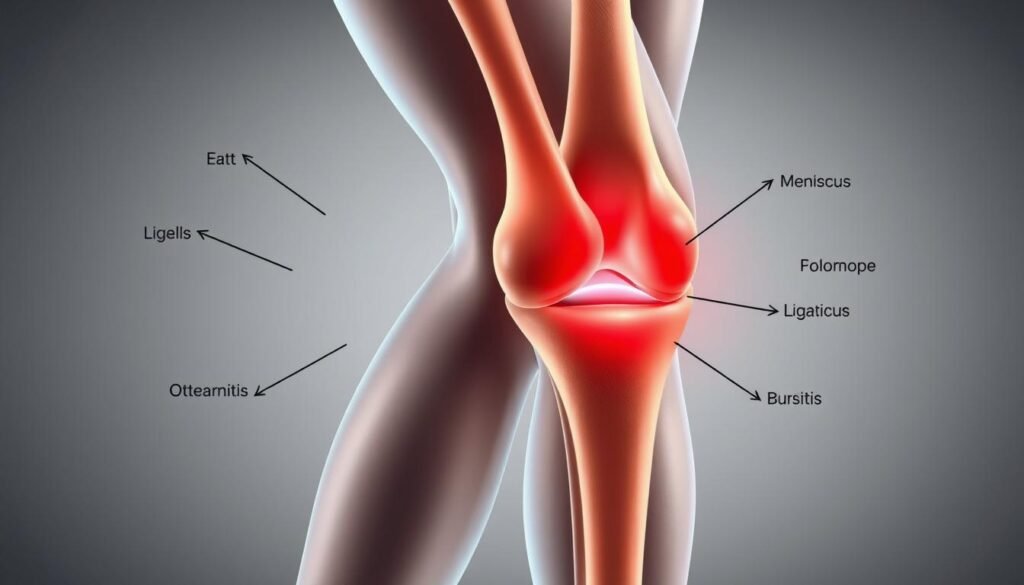
Inflammatory Conditions and Degenerative Joint Disease
Persistent swelling often points to inflammatory arthritis like rheumatoid disease. Unlike acute injuries, these conditions cause morning stiffness lasting over 30 minutes. Degenerative changes, such as cartilage loss in osteoarthritis, may coexist with meniscus tears—a combination requiring tailored management.
Key indicators include:
- Gradual onset of discomfort during weight-bearing activities
- Joint space narrowing visible on X-rays
- Limited response to anti-inflammatory medications
Pes Anserine Bursitis and Medial Plica Syndrome
Localized tenderness below the joint line often signals pes anserine bursitis. This inflammation mimics ligament injuries but responds better to targeted therapies. Meanwhile, thickened synovial folds (plica) can snap during movement, creating sharp, recurrent pain.
We differentiate these syndromes through:
- Palpation of specific anatomical landmarks
- Pain patterns during knee flexion tests
- Absence of mechanical locking seen in meniscus issues
Accurate diagnosis prevents unnecessary interventions. A 2022 study found 38% of chronic inner-joint complaints stemmed from overlooked plica complications.
Clinical Evaluation and Physical Examination Techniques
A precise clinical evaluation transforms vague symptoms into actionable insights. We start by merging patient narratives with hands-on assessments, creating a roadmap that reveals hidden patterns. This dual approach separates transient discomfort from persistent conditions needing targeted treatment.

Comprehensive History and Symptom Analysis
We prioritize understanding how injuries began. Was it a sudden twist during sports, or did discomfort creep in after months of repetitive motion? Timing matters—acute trauma often leaves immediate swelling, while overuse issues build gradually. Patients describe sensations like “catching” or “grinding,” clues pointing to specific structures.
Comparing both sides during movement tests uncovers asymmetries. For example, limited flexion on the affected side may signal MCL involvement. We also explore prior interventions—did rest ease symptoms, or did they persist despite medication?
Special Provocative Tests and Palpation Methods
Physical exams turn theories into evidence. The valgus stress test stresses the MCL, revealing laxity when the ligament is compromised. We palpate along the joint line, noting tender spots that align with meniscal injuries or bursal inflammation.
Functional tests like squatting or stair-climbing replicate real-world strain. Responses guide treatment paths—a positive McMurray test often warrants imaging, while localized swelling might respond to corticosteroid injections. By correlating exam findings with history, we avoid overlooking subtle conditions.
Imaging, Laboratory Tests, and Diagnostic Procedures
Modern diagnostic tools bridge the gap between symptoms and actionable insights. Imaging studies and lab work transform clinical hunches into evidence-based conclusions, guiding targeted care plans.
Radiographic and MRI Insights
X-rays reveal bone alignment and joint space narrowing, crucial for detecting arthritis. But when soft tissues demand scrutiny, MRI steps in. This advanced scan captures ligaments, cartilage, and fluid buildup with precision—key for confirming tears or inflammation missed by basic imaging.
Ultrasound shines in evaluating anserine bursitis. Its real-time imaging shows thickened bursal walls and fluid accumulation. Paired with pressure applied during exams, it helps differentiate bursitis from tendon injuries.
- MRI confirms meniscal damage and ligament integrity
- Ultrasound pinpoints bursitis without radiation exposure
- Blood tests rule out systemic inflammation in persistent cases
These tools don’t operate in isolation. A 2023 article highlighted how combining MRI findings with physical exams improved therapy accuracy by 41%. For example, surgical decisions hinge on imaging-confirmed ligament rupture severity.
Lab tests like CRP levels support diagnoses when infections or autoimmune conditions mimic mechanical injuries. Together, these methods create a diagnostic mosaic—each piece refining the clinical picture.
Management Strategies and Treatment Options
Effective treatment begins with matching interventions to the root problem. Whether stemming from repetitive strain or sudden injury, addressing inner-joint issues demands tailored approaches. We prioritize methods that restore function while minimizing downtime.
Conservative Therapies and Activity Modifications
Initial care focuses on reducing strain. Adjusting physical activity levels and incorporating rest periods often alleviates discomfort. Physical therapy strengthens supporting muscles, improving joint stability without invasive measures.
For persistent swelling, corticosteroid injections may provide relief. A 2023 study showed 68% of patients improved with structured rehab programs. “Consistency matters more than intensity during early recovery phases,” notes Dr. Ellen Torres, a sports medicine specialist.
Surgical Considerations and Advanced Interventions
When cartilage tears or ligament damage persists, surgery becomes necessary. Arthroscopic procedures repair meniscal injuries, while reconstruction restores compromised ligaments. MRI scans guide these decisions by detailing tissue integrity.
Postoperative rehab emphasizes gradual mobility restoration. Most patients resume light activities within 6-8 weeks, though full recovery may take months. Combining surgical precision with personalized rehab plans yields optimal long-term outcomes.
Integrative Approaches: Applying the “Rules of Four” in Knee Assessment
Clinicians often face time constraints when evaluating complex joint complaints. The “Rules of Four” framework simplifies this process by dividing assessments into four anatomical zones. This method ensures no critical structure goes unexamined, particularly when addressing inner-leg discomfort.
Systematic Examination Guidelines
Each quadrant corresponds to specific tissues. For example, the inner zone focuses on the medial collateral ligament and tendons. Palpating these areas reveals tenderness patterns linked to injuries or inflammation.
When instability is detected, we prioritize stress tests. A lax medial collateral complex often correlates with chronic overuse or past trauma. Simultaneously, we check for pes anserine bursitis by applying pressure below the joint line—a common cause of localized swelling.
Adapting Evaluation for Diverse Patient Profiles
Active adults may present with sports-related ligament strains, while older patients often show degenerative changes. The same four-zone approach accommodates these differences. For instance, younger athletes might require dynamic movement analysis, whereas seniors benefit from seated assessments.
Identifying anserine bursitis involves comparing bilateral tenderness. This condition frequently mimics medial collateral ligament instability, making precise palpation essential. By methodically ruling out each potential cause, we reduce diagnostic uncertainty across age groups and activity levels.
Final Insights on Navigating Your Medial Knee Pain Journey
Navigating inner-joint discomfort requires patience and precision. A systematic approach—combining detailed history with hands-on exams—remains vital. Clinicians assess aspect knee findings to uncover hidden patterns, while patients share crucial clues about symptom progression.
Key distinctions emerge through ligament evaluations and injury timelines. For example, athletes often benefit from tailored MCL injury recovery strategies based on activity demands. Even subtle aspect knee tenderness can signal specific conditions needing targeted care.
Diagnosis takes time, balancing imaging insights with functional tests. Open communication ensures both parties address all factors—from initial swelling to rehab milestones. Whether managing acute trauma or chronic strain, clarity guides every step toward lasting joint health.
