What if the sharp ache in your knee isn’t just a simple strain but a sign of something more complex? Knee discomfort often leaves people guessing—Is it the ligament? The cartilage? Or something else entirely? Understanding the source of your pain is critical, yet many struggle to differentiate between common injuries like cartilage damage and ligament strains.
The knee relies on a delicate balance of structures to function smoothly. Ligaments stabilize joints during movement, while cartilage cushions impact. When injuries occur, symptoms can overlap, creating confusion. For example, inner knee instability might suggest ligament stress, whereas a “locking” sensation could point to cartilage issues.
Accurate diagnosis shapes recovery. Misjudging the injury might delay healing or worsen damage. We’ll break down key differences in how these problems manifest, from pain patterns to mobility changes. Our insights draw from leading sports medicine research to help you navigate treatment options confidently.
Key Takeaways
- Knee injuries often involve distinct structures requiring tailored care.
- Cartilage damage may cause joint locking; ligament strains lead to instability.
- Inner knee pain typically signals ligament involvement.
- Diagnosis relies on physical exams and imaging for precision.
- Early intervention improves outcomes for both types of injuries.
- Treatment varies from rest to surgery based on severity.
Introduction to Knee Injuries
Your knee’s complex structure makes it vulnerable during sports and daily tasks. This joint combines bones, ligaments, and cartilage working in harmony. When one component fails, mobility suffers—whether from sudden twists or repetitive stress.
Two primary factors drive knee problems: acute trauma and overuse. A collision during football or awkward landing in basketball typifies sudden damage. Conversely, runners or cyclists might develop issues gradually from repeated strain.
Sports medicine experts emphasize early evaluation for precise care. Swelling or stiffness often hints at deeper trouble. Consider these common patterns:
| Injury Type | Common Causes | Key Symptoms |
|---|---|---|
| Acute Trauma | Direct impact, sudden twists | Immediate swelling, instability |
| Overuse | Repetitive motions | Gradual knee pain, stiffness |
Diagnosis starts with identifying whether the issue stems from ligaments or cartilage. While some injuries heal with rest, others demand targeted therapies. We prioritize clarity to match treatments to root causes—like distinguishing tissue tears from strained fibers.
Recovery hinges on accurate classification. A tailored plan reduces downtime and prevents recurring damage. Always consult professionals when movements feel restricted or painful.
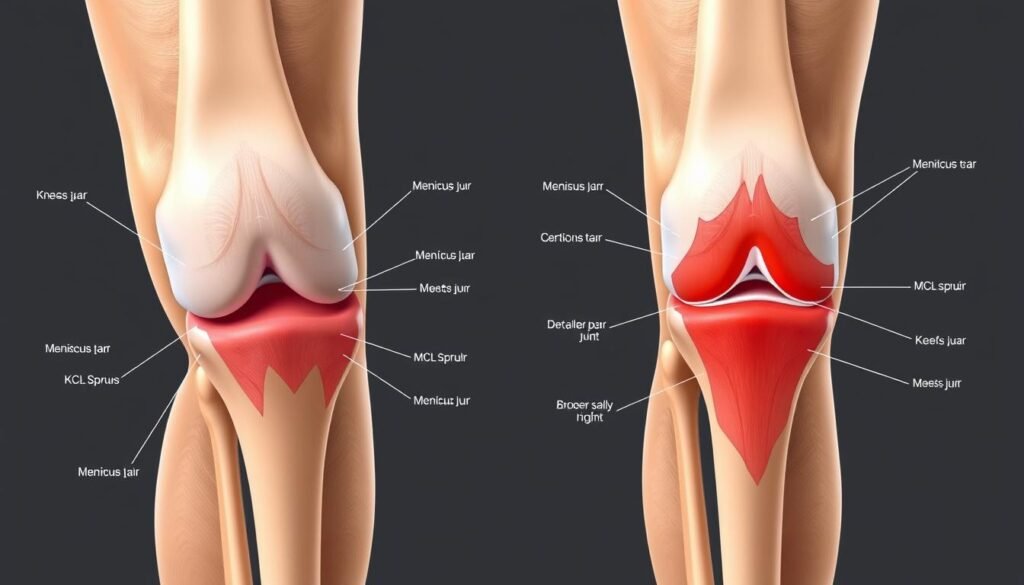
Anatomy of the Knee: Ligaments and Menisci
Your knee isn’t just a hinge—it’s a marvel of biological engineering. Bones, soft tissues, and protective structures work together to handle everything from sprinting to stair climbing. Let’s explore the critical components that keep this joint functional.
Key Knee Structures and Their Functions
The knee relies on four primary ligaments for stability. The medial collateral ligament (MCL) runs along the inner side, preventing excessive sideways motion. Paired with the collateral ligament on the outer edge, these bands act like seatbelts during lateral movements.

Between the thigh and shin bones lie two crescent-shaped cushions—the menisci. These act as shock absorbers, distributing weight evenly across the joint. Without them, everyday activities like walking would grind bone against bone.
The Role of the MCL and Meniscus in Stability
When the MCL is healthy, it stabilizes the knee during side-to-side actions. Sports medicine studies show this ligament absorbs up to 80% of valgus stress during pivots. Damage here often leads to a wobbly sensation, as detailed in our guide to common knee injuries.
Surrounding muscles like the quadriceps and hamstrings reinforce these passive structures. Strong muscles reduce strain on ligaments and cartilage, creating a protective synergy. Weakness here can tip the balance toward instability or injury.
Understanding this anatomy clarifies why targeted care matters. Each structure plays a distinct role in maintaining pain-free motion—and why diagnostics must pinpoint exactly what’s compromised.
Meniscus tear symptoms vs MCL sprain: Distinct Signs and Symptoms
How can you tell if your knee problem stems from damaged cartilage or a strained ligament? Both issues share overlapping features but require distinct management strategies. Let’s explore the markers that set them apart.
Location and Quality of Discomfort
Cartilage damage often causes sharp pain along joint lines, especially during twisting motions. Patients frequently report a “catching” sensation when extending their leg. In contrast, ligament strains produce tenderness concentrated on the inner knee area.
| Feature | Cartilage Issue | Ligament Strain |
|---|---|---|
| Swelling Timing | Develops over 24 hours | Appears immediately |
| Motion Impact | Locking during rotation | Stiffness when bending |
| Weight-Bearing | Pain worsens with squatting | Discomfort eases when still |
Decoding Initial Warning Signs
A sudden pop during activity often signals tissue damage in cartilage-related injuries. MCL strains typically lack this audible cue but create instability when shifting directions. Both conditions may limit range of motion, though through different mechanisms.
“The absence of immediate swelling doesn’t rule out significant damage—delayed inflammation often accompanies cartilage tears,” notes a 2023 Johns Hopkins Sports Medicine study.
While instability occurs in both scenarios, its triggers differ. Cartilage problems cause mechanical slippage, while ligament issues lead to muscular compensation. Recognizing these patterns helps athletes seek appropriate care faster.
Common Causes of Knee Injuries in Sports
Athletes push their limits daily, but what forces put their knees at risk? Sports-related injuries often stem from three primary triggers: sudden collisions, awkward pivots, and repetitive strain. These mechanisms disrupt the joint’s delicate balance, leading to pain or instability.

Impact, Twisting, and Overuse Mechanisms
High-impact activities like football tackles deliver forceful blows to the knee. Such collisions strain ligaments and compress cartilage. A 2022 study in the Journal of Athletic Training found that 43% of contact sport injuries involve direct trauma to the joint.
Twisting motions during soccer or basketball create rotational stress. Quick direction changes overload tissues not designed for lateral force. Overuse from running or cycling wears down structures gradually, often causing subtle damage before major symptoms appear.
| Mechanism | Common Sports | Prevention Tips |
|---|---|---|
| Impact | Football, rugby | Strengthen quadriceps |
| Twisting | Soccer, tennis | Improve pivot control |
| Overuse | Running, cycling | Adjust training intensity |
Sports medicine professionals emphasize tailored conditioning programs. These reduce injury risks by addressing muscle imbalances and movement patterns. Proper technique during activities also lowers strain on vulnerable areas.
“Prehab exercises targeting knee stability cut injury rates by 28% in collegiate athletes,” reports a 2023 sports medicine review.
Understanding these causes helps athletes and trainers build safer routines. Next, we’ll explore how experts pinpoint specific damage through advanced diagnostics.
Diagnostic Methods and Imaging for Knee Injuries
Accurate identification of knee issues starts with thorough assessments. Doctors combine hands-on evaluations with advanced technology to pinpoint damage. This approach minimizes guesswork and tailors care to each patient’s needs.
Physical Examinations and Patient History
Healthcare providers begin by asking about injury mechanisms and pain patterns. They check for tenderness along the inside knee or joint line—key markers for ligament or cartilage problems. Simple movement tests often reveal instability or restricted motion.
For example, pressing on the medial collateral ligament area helps assess MCL integrity. Rotation tests may expose cartilage irregularities. These findings guide decisions about further imaging.
The Role of MRI and Other Imaging Techniques
When physical exams suggest structural damage, MRI scans provide detailed visuals of soft tissues. This technology detects subtle tears in ligaments or cartilage that X-rays miss. Ultrasound and CT scans complement MRIs in specific cases.
| Imaging Modality | Best For | Limitations |
|---|---|---|
| MRI | Soft tissue detail | Cost, availability |
| X-ray | Bone fractures | Poor ligament visibility |
| Ultrasound | Dynamic assessment | Operator-dependent |
Combining these methods creates a complete picture of the knee joint. Early, precise diagnosis helps avoid unnecessary surgery or prolonged recovery. As one orthopedic specialist notes: “Imaging confirms what our hands tell us—it’s teamwork between art and science.”
Treatment Options for Meniscus Tears
Modern approaches to joint care prioritize minimally invasive solutions. Many patients achieve full recovery through structured programs that combine immediate care with gradual strengthening.
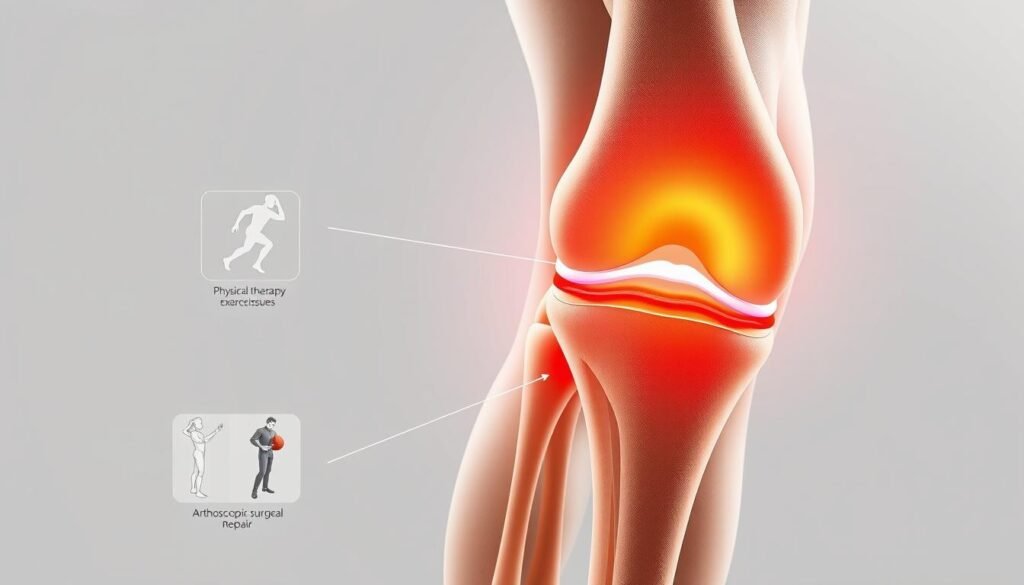
Healing Through Conservative Care
The R.I.C.E. protocol remains foundational for acute injuries. Rest prevents further damage, while compression wraps minimize swelling. Applying ice for 15-minute intervals reduces inflammation effectively.
Targeted physical therapy rebuilds muscle support around the joint. Therapists focus on exercises that improve flexibility without straining healing tissues. A 2023 study in Clinical Orthopaedics found 68% of partial-thickness injuries healed completely with this approach.
- Anti-inflammatory medicine like NSAIDs manages discomfort
- Elevation accelerates fluid drainage
- Custom braces provide stability during recovery
“Early movement within pain limits preserves joint function better than prolonged immobilization,” states the American Academy of Orthopaedic Surgeons.
Most cases avoid surgery when addressed promptly. Regular progress checks ensure therapies adapt to changing needs. This strategy helps patients return to daily activities while protecting long-term knee health.
Managing MCL Sprain with Conservative Care
Most ligament strains respond well to non-surgical methods when addressed promptly. For issues involving the medial collateral ligament, a structured conservative approach often restores stability without invasive procedures. Early intervention minimizes complications and accelerates recovery timelines.
Rest and Bracing Techniques
Initial treatment focuses on reducing stress to the inner knee. A hinged brace provides external support, limiting sideways motion while allowing controlled bending. This protects healing fibers during daily activities. Doctors typically recommend 2-4 weeks of restricted movement paired with elevation to manage swelling.
Three phases guide recovery:
- Phase 1: Restrict weight-bearing and use ice therapy
- Phase 2: Introduce gentle range-of-motion exercises
- Phase 3: Strengthen surrounding muscles with resistance bands
Physical Therapy’s Role in Recovery
Targeted exercises rebuild strength without overloading damaged tissues. Therapists emphasize hamstring and quadriceps activation to compensate for ligament weakness. A 2023 Journal of Orthopaedic & Sports Physical Therapy study found patients completing structured programs regained 92% of pre-injury mobility within eight weeks.
“Conservative care succeeds when patients commit to gradual progression—rushing rehabilitation risks reinjury,” advises Dr. Elena Torres, a leading sports physiotherapist.
While severe cases may require surgery, most MCL injuries heal completely through these methods. Regular monitoring ensures therapies adapt as stability improves, safeguarding long-term joint health.
Surgical Interventions: When Is Surgery Needed?
When do knee problems require more than rest and rehabilitation? Surgery becomes essential when conservative treatments fail to restore stability or relieve persistent discomfort. Structural damage that limits daily function often demands precise intervention to prevent long-term complications.
Arthroscopy and Other Minimally Invasive Procedures
Arthroscopic techniques allow surgeons to repair damaged tissues through tiny incisions. This approach reduces recovery time compared to traditional open procedures. Common candidates include:
- Patients with complete ligament ruptures causing joint instability
- Cases where cartilage fragments impede normal movement
- Persistent instability despite months of physical therapy
Advanced imaging guides surgical planning, ensuring repairs target specific problem areas. A 2023 Journal of Bone & Joint Surgery study found arthroscopy patients resumed light activities 40% faster than those undergoing open surgery.
“Minimally invasive methods preserve healthy tissue while addressing critical damage—this precision accelerates healing,” explains Dr. Rachel Nguyen, orthopedic surgeon at Mayo Clinic.
Recovery typically spans 6-12 weeks, depending on injury severity. Postoperative care includes bracing and progressive exercises to rebuild strength. While not every case requires going under the knife, timely surgical assessment can prevent irreversible joint deterioration.
Rehabilitation and Physical Therapy Insights
Effective rehabilitation bridges the gap between injury and full mobility. Every recovery journey demands a strategy as unique as the individual—no two programs look identical. Tailored approaches address specific weaknesses while respecting healing timelines.
Developing a Customized Recovery Program
Physical therapists design plans based on injury severity and lifestyle goals. A runner with cartilage damage needs different exercises than a construction worker recovering from ligament strain. Initial sessions focus on reducing swelling and restoring basic range motion.
Three phases structure most programs:
| Phase | Weeks | Focus |
|---|---|---|
| 1: Protection | 1-3 | Reduce inflammation, gentle movement |
| 2: Strengthening | 4-6 | Rebuild muscle, improve stability |
| 3: Functional Training | 7+ | Sport-specific drills, endurance |
Recovery time varies widely. Minor ligament strains may resolve in four weeks, while complex cases require months. Therapists adjust intensity weekly, using feedback to prevent setbacks.
“Custom plans improve outcomes by 40% compared to generic protocols,” states a 2023 Journal of Orthopaedic Research meta-analysis.
Ongoing evaluations track progress in knee mechanics and strength. This data-driven approach ensures each phase builds toward lasting joint health. Consistent effort during therapy often determines long-term success.
Comparative Recovery Timelines of Knee Injuries
Recovery expectations after knee damage vary dramatically based on affected structures. While some injuries resolve within weeks, others demand months of careful rehabilitation. Let’s break down typical healing periods for common joint issues.
- Medial collateral ligament strains: 4-8 weeks with proper bracing
- Cartilage injuries: 6-12 weeks for partial tears
- ACL ruptures: 6-12 months post-surgery
Three factors heavily influence timelines:
- Severity of tissue damage
- Consistency with physical therapy
- Age and overall joint health
Athletes often recover faster than sedentary individuals due to stronger supporting muscles. For example, a professional athlete with an MCL injury might return in 5 weeks through intensive rehab. Meanwhile, older adults with similar damage could need 10 weeks.
“Grade 1 ligament injuries heal 60% faster than Grade 3 tears when treated early,” states a 2023 University of Colorado Sports Medicine report.
Understanding these benchmarks helps patients set realistic goals. Always consult specialists to tailor recovery plans to your unique situation.
Prevention Strategies for Maintaining Knee Health
Protecting your knees starts long before discomfort appears—proactive care keeps joints resilient. We prioritize strategies that shield the inside knee and surrounding structures from daily wear. Simple habits build defenses against common injuries linked to sports and repetitive motions.
Strengthening the thigh muscles creates natural armor for your knees. Squats and lunges target quadriceps that stabilize the MCL during lateral movements. Balance exercises, like single-leg stands, improve coordination to prevent awkward twists.
Proper warm-ups prepare tissues for action. Dynamic stretches increase blood flow to the side ligaments and tendons. A 2023 study in Sports Health found athletes who warmed up reduced inside knee injuries by 37% compared to those who skipped this step.
“Consistent conditioning programs act like insurance policies for joints—they pay dividends during high-stress moments,” advises Dr. Marcus Wheeler, orthopedic specialist at Stanford Medicine.
In football and similar activities, technique matters. Pivoting with bent knees lowers strain on the MCL. Coaches emphasize keeping hips aligned over feet during cuts to avoid overloading one inside knee. Pair these methods with rest days to let tissues recover fully.
Finally, maintain flexibility through yoga or foam rolling. Tight muscles pull joints out of alignment, increasing injury risks. Small daily efforts compound into lasting protection for your most hardworking joints.
When to Seek Expert Sports Medicine Guidance
Ignoring persistent knee discomfort could turn a manageable issue into a long-term problem. While minor aches often resolve with rest, certain patterns demand professional evaluation. Timing matters—delaying care for complex injuries risks prolonged recovery or irreversible joint damage.
Recognizing Warning Signs and Early Intervention
Three red flags signal the need for expert assessment:
- Persistent swelling lasting over 48 hours despite ice and elevation
- Difficulty bearing weight on the affected leg
- Audible popping sounds during movement
Sports medicine specialists use advanced techniques to pinpoint issues that self-care can’t address. For example, lingering instability in the inside knee area often indicates MCL tears requiring targeted rehabilitation. A 2023 Johns Hopkins study found patients who sought care within 72 hours of injury recovered 33% faster than those who waited.
“Early diagnosis transforms outcomes—it’s the difference between a six-week recovery and six months of setbacks,” emphasizes Dr. Laura Simmons from the American Academy of Sports Medicine.
When conservative measures fail to resolve knee pain, surgical options might become necessary. Specialists tailor plans based on activity levels and damage severity, whether for weekend warriors or professional athletes. Don’t gamble with mobility—expert guidance ensures your treatment matches your body’s needs.
Final Reflections on Knee Health
Understanding knee health begins with recognizing the distinct roles of its structures. While cartilage cushions impact, ligaments like the medial collateral provide stability during movement. Differentiating between tissue damage types ensures proper care—whether addressing sudden instability or gradual stiffness.
Early evaluation by sports medicine experts remains critical. Minor issues often resolve with rest and bracing, but severe cases may require determining if MCL surgery is right for. Tailored plans combining therapy and muscle conditioning accelerate recovery while preventing reinjury.
Maintaining joint resilience involves proactive steps. Strengthening thigh muscles supports the collateral ligament during pivots, while balance drills improve control. Regular assessments catch subtle changes before they escalate, especially for active individuals.
Persistent discomfort warrants professional insight. Specialists decode complex symptoms, guiding patients through conservative or surgical pathways. Prioritizing knee health today safeguards mobility for tomorrow’s challenges.
