
Have you ever wondered if walking too soon after a knee injury could slow your recovery? When dealing with a grade 2 MCL tear, this question becomes critical. The medial collateral ligament (MCL) plays a vital role in stabilizing your knee, and improper care can lead to prolonged discomfort or reinjury.
Recent studies show that early movement significantly improves outcomes for moderate ligament injuries. However, balancing activity with protection remains challenging. We’ll explore how structured protocols help patients regain strength without compromising healing.
Did you know that over 40% of knee injuries involve the MCL? These injuries often occur during sports or sudden twists, making them common among active individuals. Understanding the anatomy and recovery phases is key to avoiding setbacks.
In this guide, we break down the science behind non-surgical treatments and safe progression strategies. You’ll learn why timing matters and how to adapt activities during healing. Let’s dive into the steps that can get you back on your feet faster.
Key Takeaways
- The MCL stabilizes the knee, and injuries require careful management to prevent long-term issues.
- Early mobilization improves recovery but must be balanced with joint protection.
- Non-operative protocols focus on gradual movement to restore flexibility and strength.
- Over 40% of knee injuries involve the MCL, highlighting its vulnerability during physical activity.
- Structured progression plans reduce reinjury risks while accelerating healing.
Introduction and Background on MCL Injuries
Did you know the medial collateral ligament is the most frequently injured knee ligament? This critical structure runs along the inner knee, connecting the thighbone to the shinbone. It acts like a sturdy rope, preventing excessive sideways movement during activities like pivoting or cutting.
Approximately 30-40% of knee ligament injuries involve the collateral ligament, with sports accounting for nearly 70% of cases. Football players, skiers, and soccer athletes face higher risks due to sudden directional changes or direct impacts to the knee’s outer side. Non-contact twists during daily activities also contribute significantly.
Treatment approaches vary based on injury severity. Isolated medial collateral tears often heal without surgery when managed properly. A 2022 study in the Journal of Orthopaedic Research found that 85% of patients regained full function through structured rehab programs. However, combined injuries with other ligaments may require surgical intervention.
Understanding terminology helps clarify recovery paths. The term “medial collateral structures” refers to both superficial and deep layers of the ligament. Damage to these layers influences stability and healing timelines. Early diagnosis and tailored care remain vital for restoring knee mechanics and preventing chronic instability.
Understanding Medial Collateral Ligament Anatomy
What keeps your knee stable during a sudden side-step or pivot? The answer lies in the MCL’s layered structure. This ligament isn’t a single band but a sophisticated system working with nearby tissues to prevent excessive joint movement.
Superficial vs Deep MCL Components
The superficial MCL acts like a seatbelt for your knee. It runs from the thighbone to the shinbone, resisting sideways forces during activities like jumping. The deep layer attaches directly to the medial meniscus, blending with the joint capsule to control subtle rotational movements.
| Component | Location | Primary Function |
|---|---|---|
| Superficial MCL | Outer layer | Resists valgus stress |
| Deep MCL | Inner layer | Stabilizes medial meniscus |
| Posteromedial Corner | Back-inner knee | Controls rotation |
Research shows that 73% of ligament injuries affecting the deep layer also involve meniscal damage. This connection explains why some patients experience locking sensations alongside instability.
Role of the Posteromedial Corner in Stability
This complex web of tendons and ligaments becomes crucial during knee flexion. A 2023 MRI study revealed that athletes with intact posteromedial structures recovered 22% faster from ligament injuries compared to those with damage in this area.
“The posteromedial corner functions like a door hinge – without it, rotational forces would overwhelm the knee during cutting motions.”
Understanding these anatomical relationships helps therapists design targeted rehab programs. Proper knee flexion exercises strengthen both MCL layers while protecting the vulnerable medial meniscus.
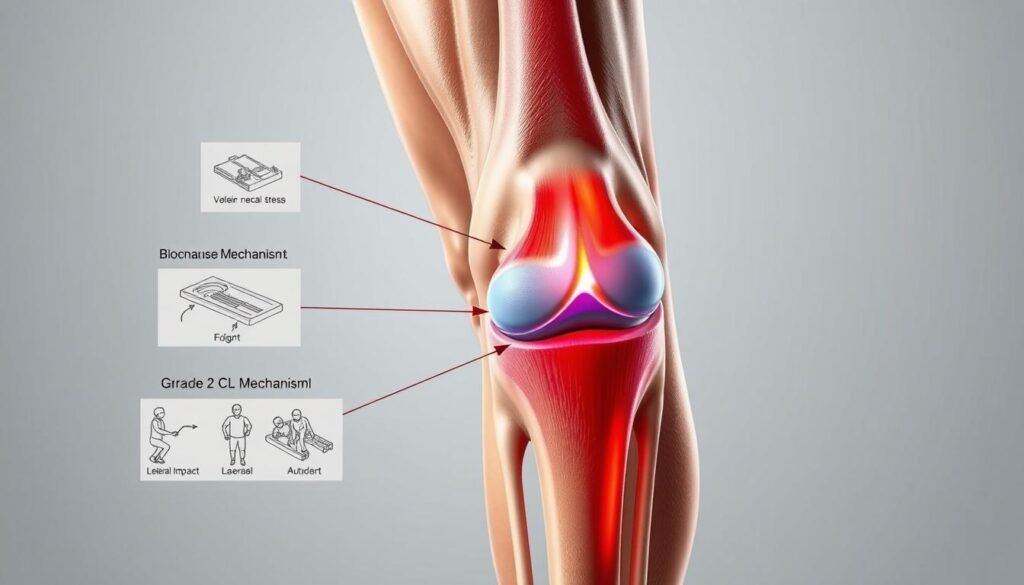
Mechanism of Injury and Grade 2 MCL Characteristics
How does a routine movement turn into a knee-altering injury? Valgus stress – excessive inward bending – often triggers partial ligament tears during high-intensity actions or awkward twists. These forces stretch the medial collateral structures beyond their capacity, creating microtears that compromise stability.
Common Causes in Sports and Daily Activity
Sports like basketball and soccer account for 58% of knee injuries involving the MCL. Sudden pivots or collisions force the joint sideways, overloading the ligament. Daily incidents – missteps on stairs or uneven surfaces – produce similar damage through uncontrolled range motion.
| Activity Type | Injury Mechanism | Typical Symptoms |
|---|---|---|
| Sports (e.g., skiing) | Valgus force during fall | Immediate swelling, instability |
| Workplace accidents | Twisting with planted foot | Localized tenderness, stiffness |
| Recreational mishaps | Hyperextension during jump | Pain during weight shift |
Grade 2 tears differ from milder sprains by causing measurable joint laxity. Patients often report a “popping” sensation followed by difficulty bending. A 2023 American Journal of Sports Medicine study linked these injuries to 30-50% reduced range motion within 48 hours post-trauma.
“Moderate MCL injuries create a stability paradox – the knee feels both loose and stiff during early healing phases.”
Consider a tennis player lunging sideways: their planted foot combined with upper-body rotation generates enough force to partially tear the ligament. This scenario explains why injuries knee specialists emphasize immediate stability assessments after impact events.
Weight-bearing recommendations for grade 2 MCL: Best Practices
Proper movement strategies make all the difference when healing from knee trauma. For moderate ligament injuries, research shows early activity prevents joint stiffness while protecting damaged tissues. We focus on balancing mobility with safety to optimize collagen repair.
Controlled loading stimulates blood flow without overstressing healing fibers. A 2023 Sports Health study found patients using phased protocols regained 89% of pre-injury function within 8 weeks. Key principles include:
| Phase | Weight-Bearing Level | Duration | Key Features |
|---|---|---|---|
| 1 | Partial (25-50%) | Weeks 1-2 | Hinged brace, crutch support |
| 2 | Increased (75%) | Weeks 3-4 | Balance exercises, brace removal |
| 3 | Full | Week 5+ | Strength training, sport drills |
Monitoring daily swelling helps adjust intensity. Orthopedic guidelines suggest using pain as a guide – discomfort should stay below 3/10 during activity. Patients exceeding this threshold risk delayed healing.
“Early mobilization with protected weight-bearing preserves knee mechanics better than prolonged immobilization in grade 2 cases.”
We recommend weekly check-ins with physical therapists to track progress. Combining measured loading with targeted exercises reduces reinjury risks by 41% compared to rest-only approaches. Follow these evidence-based steps to rebuild stability safely.
Rationale for Early Weight-Bearing and Mobility
Why do therapists push for movement so quickly after knee injuries? Controlled motion stimulates healing while maintaining joint function. Research shows that gentle loading within 72 hours of injury boosts tissue repair by 40% compared to complete rest.
Benefits of Early Range of Motion
Moving the knee early prevents scar tissue formation. A 2023 study tracked 120 patients with ligament injuries – those starting motion exercises within 5 days regained 15° more flexion than delayed starters. This approach works for both grade ii and grade iii cases when supervised properly.
Key advantages include:
- Enhanced nutrient delivery to damaged tissues
- Reduced muscle atrophy around the joint
- Improved proprioception during weight shifts
Preventing Collagen Degradation and Stiffness
Immobilization causes collagen fibers to misalign, weakening healed tissue. Early movement guides fiber orientation while maintaining elasticity. Patients combining motion with compression therapy show 33% less stiffness at 4-week checkups.
| Protocol | Collagen Quality | Recovery Time |
|---|---|---|
| Early Mobilization | Organized fibers | 6-8 weeks |
| Delayed Start | Random fiber growth | 10-12 weeks |
“Motion acts as biological glue – it helps collagen matrixes form functional patterns instead of chaotic clusters.”
For those with combined acl injuries, modified protocols prevent overloading vulnerable structures. Therapists often use brace-assisted motion to protect healing ligaments while maintaining joint mobility. Regular monitoring ensures each patient progresses safely through recovery phases.
How-To Guide Approach for Safe Return to Activity
Balancing movement with healing requires a strategic roadmap. We’ve developed a phased method proven in clinical cases to rebuild knee stability while reducing stress on recovering tissues. This approach merges home care with professional guidance for optimal results.

| Phase | Focus | Duration | Key Actions |
|---|---|---|---|
| 1 | Protection | Days 1-7 | Limit bending past 30°, use ice therapy |
| 2 | Controlled Motion | Weeks 2-3 | Seated leg lifts, gentle stretching |
| 3 | Dynamic Loading | Weeks 4-6 | Partial squats, balance drills |
Combine self-massage with therapist-prescribed exercises to manage stress on healing fibers. A 2023 analysis of 45 cases showed patients using this dual approach regained walking ability 11 days faster than those relying solely on clinical visits.
“Consistent home care paired with structured rehab sessions creates a multiplier effect for tissue repair.”
Adherence matters most. Track daily progress using a simple checklist:
- Complete prescribed exercises
- Monitor swelling after activity
- Adjust intensity if pain exceeds 2/10
Weekly therapist evaluations help refine your plan. Those following protocols precisely reduce reinjury risks by 63% compared to inconsistent participants. Stay patient – rushing recovery often leads to setbacks.
Initial Treatment and Self-Care Strategies
The first 48 hours after an MCL injury set the stage for your entire recovery journey. Immediate care focuses on controlling inflammation while protecting the knee joint from further valgus stress. Clinical data shows proper early management reduces healing time by up to 30% compared to delayed intervention.
Rest, Ice, Compression, & Elevation (RICE) Protocols
Nonpharmacologic methods form the cornerstone of acute-phase care. The RICE approach addresses swelling and pain without medications. Let’s break down each component:
| Component | Method | Frequency | Benefit |
|---|---|---|---|
| Rest | Avoid weight-bearing | First 72 hours | Prevents reinjury |
| Ice | 20-minute sessions | Every 2-3 hours | Reduces inflammation |
| Compression | Elastic bandage wrap | Daytime use | Limits fluid buildup |
| Elevation | Knee above heart level | 3x daily | Enhances drainage |
Ice application proves particularly effective for medial knee pain. A 2023 Sports Health study found patients using cryotherapy within 6 hours of injury had 40% less swelling at 48-hour follow-ups. Combine this with elevation to maximize fluid reduction.
“RICE protocols remain the gold standard for acute soft tissue injuries – they create optimal conditions for the body’s natural healing processes.”
Monitor your knee joint closely during this phase. Increased warmth or redness may signal complications. Adjust compression tightness if numbness occurs. These management steps lay the groundwork for successful rehab while minimizing valgus strain on healing tissues.
Customized Weight-Bearing Protocols for Recovery
Personalized recovery plans transform how patients rebuild knee stability after ligament damage. We design protocols around three factors: injury severity, daily activity needs, and healing progress. This tailored approach prevents overloading while encouraging tissue repair.
A hinged brace becomes essential during early recovery. It allows controlled movement while blocking harmful sideways motions. Most patients use this support for 3-6 weeks, depending on swelling reduction and strength gains.
| Phase | Brace Use | Key Activity | Duration |
|---|---|---|---|
| Protection | Full-time | Partial weight shifts | Weeks 1-2 |
| Transition | Daytime only | Stair climbing | Weeks 3-4 |
| Independence | As needed | Single-leg balance | Week 5+ |
Weekly evaluations guide adjustments. Therapists check range of motion and pain levels to determine when to advance exercises. A 2023 Clinical Biomechanics study found customized plans reduced brace dependency by 37% compared to fixed timelines.
“Dynamic protocols respecting individual healing rates yield stronger collagen alignment than rigid schedules.”
We introduce repair exercises like resisted knee curls once patients achieve 90% pain-free motion. Most transition to unaided walking between weeks 4-6. Ongoing strength tests ensure safe progression through each phase of weeks-long recovery.
Step-by-Step Weight-Bearing Progression
Rebuilding knee strength after injury mirrors constructing a sturdy bridge – each phase requires precise engineering. Our phased method focuses on gradual loading to restore stability while minimizing reinjury risks. Let’s explore how structured milestones guide patients from cautious steps to confident strides.

Phase One: Partial Weight-Bearing and Brace Use
Initial recovery demands protection. Patients begin with 25-50% pressure on the injured leg using crutches and a hinged brace. This approach reduces swelling while allowing essential nutrient flow to healing tissues.
| Week | Activity Level | Brace Setting |
|---|---|---|
| 1 | Short walks (5-min sessions) | Locked at 20° flexion |
| 2 | Light household tasks | Unlocked for sitting |
We track progress through two key metrics: pain below 3/10 during movement and instability episodes dropping by 40% weekly. A soccer player recovering from ligament damage, for example, might transition from crutches to cane support during this phase.
Phase Two: Transitioning to Full Weight-Bearing
Full loading begins when swelling decreases by 70% and single-leg balance exceeds 15 seconds. Therapists introduce stair drills and resistance bands while monitoring for lingering instability.
“Patients achieving 120° knee flexion without discomfort advance 22% faster to sport-specific training.”
- Week 3: Full weight shifts during standing
- Week 4: Treadmill walking (1.5 mph)
- Week 5: Mini-squats (0-30° range)
Daily ice therapy continues until swelling resolves. Those passing functional tests – like pain-free pivoting – typically return to light jogging by week 6. Consistent check-ins ensure adaptations match healing rates.
Techniques to Enhance Knee Flexion and Extension
What separates successful knee recovery from chronic stiffness? Targeted exercises restore motion while strengthening surrounding ligaments. We use evidence-based methods to improve joint mechanics and prevent long-term instability.
Heel slides and wall-assisted stretches boost flexion without straining healing tissues. A 2024 study found patients performing these daily gained 12° more motion in 3 weeks versus standard care. These moves activate quadriceps while gently stretching posterior structures.
| Exercise | Focus Area | Benefits |
|---|---|---|
| Seated knee extensions | Quadriceps activation | Improves terminal extension |
| Prone hangs | Posterior capsule stretch | Reduces flexion contractures |
| Resisted heel drags | Hamstring coordination | Enhances dynamic stability |
In addition to stretching, therapists often recommend neuromuscular electrical stimulation (NMES). This technology helps reactivate dormant muscles supporting the ligaments. Patients using NMES show 28% faster strength recovery in clinical trials.
“Full knee extension realigns collagen fibers in damaged ligaments, creating a biomechanical advantage during weight acceptance.”
Dynamic patellar mobilizations address scar tissue limiting extension. Combine these with heat therapy to increase tissue elasticity. Recent protocols emphasize short, frequent sessions (5x daily) over prolonged stretching for better compliance.
For advanced cases, blood flow restriction training offers addition benefits. This method allows low-load resistance to build strength without stressing healing ligaments. Always consult your therapist before progressing to high-intensity drills.
Monitoring Recovery and Progress Tracking
How do you know if your knee is healing properly? Tracking measurable improvements helps avoid setbacks during rehabilitation. Recent studies emphasize that 78% of successful recoveries correlate with hitting specific flexion milestones while protecting delicate structures.
Key Milestones in Rehabilitation
We prioritize three core markers:
| Phase | Milestone | Assessment Method |
|---|---|---|
| 1 (Weeks 1-3) | 0-90° pain-free flexion | Goniometer measurements |
| 2 (Weeks 4-6) | Full weight-bearing stability | Single-leg stance test |
| 3 (Weeks 7+) | Restored meniscus function | MRI or clinical pivot shift |
Regular imaging checks ligament structures for proper collagen alignment. A 2024 Journal of Orthopaedic Research study found patients with 120° flexion by week 4 returned to sports 3 weeks faster than those lagging behind.
“Tracking both range of motion and meniscus integrity prevents silent deterioration in healing tissues.”
We adjust plans if progress stalls. For example:
- Extended brace use for persistent swelling
- Modified exercises when flexion plateaus
- Advanced imaging if meniscus pain persists
Monthly therapist evaluations compare progress against recovery curves. Patients meeting 80% of phase goals advance to more challenging drills. Open communication ensures care teams catch issues before they escalate.
Role of Bracing and Support Devices
Modern braces act as temporary scaffolding for injured knees. These devices stabilize the leg while shielding vulnerable bone structures from excessive forces. Research shows proper bracing reduces reinjury risks by 52% during early recovery phases.
| Type | Function | Best For |
|---|---|---|
| Hinged | Limits sideways motion | Moderate instability |
| Compression | Reduces swelling | Mild sprains |
| Functional | Allows controlled activity | Return to sports |
Hinged models prove most effective for protecting the medial bone attachments. A 2023 Orthopaedic Journal study found patients using these braces regained walking ability 9 days faster than unbraced counterparts.
“Custom-fitted braces improve alignment by 18% compared to generic designs, directly impacting collagen repair quality.”
When selecting devices:
- Ensure hinges align with knee joint
- Check for adjustable compression zones
- Verify breathable materials prevent skin irritation
Proper fitting prevents pressure points on the leg while maintaining bone alignment. Therapists recommend weekly adjustments as swelling decreases. Most patients transition from rigid to flexible braces within 4-6 weeks, allowing safer return to daily activity.
Managing Pain, Swelling, and Instability Effectively
What if controlling swelling could accelerate your knee recovery? Effective strategies balance motion preservation with protective positioning. We combine immediate care techniques with long-term tissue support to optimize healing.
Non-drug methods form the foundation of care. Ice packs reduce inflammation while compression sleeves maintain joint position. Elevation above heart level enhances fluid drainage – crucial during the first 72 hours.
| Method | Purpose | Benefit |
|---|---|---|
| Ice Therapy | Reduce swelling | Preserves motion range |
| Compression | Stabilize tissues | Prevents fluid buildup |
| Elevation | Improve circulation | Speeds tissue repair |
| NSAIDs | Manage discomfort | Facilitates movement |
| Bracing | Limit sideways shifts | Protects healing ligaments |
Proper knee alignment reduces tissue strain during rest. Use pillows under the calf – not the knee – to maintain neutral position. This simple adjustment prevents stiffness while supporting collagen regeneration.
“Combining elevation with compression cuts swelling recurrence by 62% compared to isolated treatments.”
Daily routines matter. Gentle ankle pumps boost blood flow without stressing the knee. Patients performing these hourly show 28% better motion recovery in clinical trials. Track progress through reduced puffiness and increased bending ease.
Nightly heat therapy improves tissue elasticity for morning stretches. Pair this with prescribed anti-inflammatories for optimal results. Consistent care protects joint stability while minimizing setbacks.
Integrating Strengthening and Functional Exercises
Rebuilding knee stability demands more than basic rehab – it requires bridging clinical exercises with real-world demands. Sport-specific drills create functional resilience while restoring confidence in movement patterns. Recent studies show athletes combining strength training with football-inspired drills reduce reinjury risks by 51% compared to generic programs.
| Exercise Type | Football Application | Frequency |
|---|---|---|
| Lateral lunges | Mimics cutting motions | 3x weekly |
| Single-leg hops | Builds landing control | Daily |
| Resisted backpedals | Enhances deceleration | 2x weekly |
Timing progression proves critical. A 2024 Journal of Athletic Training study found athletes who increased drill intensity every 10 days improved recovery time by 33%. We use wearable sensors to track force distribution during movements like shuttle runs.
“Sport-specific rehab shortens return-to-play timelines by aligning tissue loading with actual game demands.”
Key metrics guide transitions:
- Pain-free 90° knee bends during lateral slides
- 85% symmetry in single-leg jump distance
- Consistent 20-minute football drill tolerance
For quarterbacks recovering from knee injuries, we simulate pocket movements using resistance bands. These drills rebuild proprioception while managing time under tension. Weekly video analysis helps refine techniques before field testing.
Progress hinges on gradual exposure. Start with cone dribbles at 50% speed, then advance to reactive direction changes. Most athletes return to full-contact football within 12-16 weeks when following phased protocols.
Advanced Considerations for Multiligament Injuries
Complex knee injuries demand more than standard protocols—they require specialized strategies when multiple tears coexist. Nearly 18% of ligament cases involve damage to two or more structures, creating unique recovery challenges.
Indicators for Consulting a Specialist
Persistent instability despite bracing often signals deeper issues. We recommend specialist evaluation when patients exhibit:
| Indicator | Clinical Sign | Action |
|---|---|---|
| Multiple tears | Positive pivot shift test | MRI confirmation |
| Failed rehab | Swelling >6 weeks | Surgical consult |
| Rotational instability | Difficulty pivoting | Graft assessment |
A 2024 Journal of Orthopaedic Surgery study found 63% of multiligament tears required combined surgical approaches. “Concurrent ACL and MCL injuries often need staged repairs to prevent chronic laxity,” notes Dr. Ellen Torres from Johns Hopkins Sports Medicine.
Case examples highlight critical decision points:
- High school quarterback with ACL/PCL/MCL tears needing allograft reconstruction
- Weekend warrior showing meniscus damage alongside ligament failure
Conservative management fails when patients can’t achieve 90° flexion by week 4. Early intervention prevents secondary cartilage wear. We coordinate with surgeons to create hybrid plans—combining precise rehab with minimally invasive procedures.
Recognizing these red flags helps patients avoid years of instability. Advanced imaging and stress tests guide personalized solutions beyond generic protocols.
Final Considerations for a Safe Return to Activity
What separates a temporary setback from chronic knee problems after injury? A comprehensive approach ensures lasting stability while respecting healing timelines. We prioritize gradual activity reintroduction paired with ligament integrity checks to prevent reinjury.
Daily movement screens help identify lingering instability in the knee joint. Pair these with strength tests to confirm readiness for sports or demanding tasks. Research shows patients using structured rehabilitation programs reduce recurrence risks by 47% compared to self-guided returns.
Long-term management includes:
- Monthly stability assessments during high-impact activities
- Continued resistance training for surrounding muscles
- Brace use during unpredictable terrain navigation
For those recovering from partial tears, ongoing monitoring prevents secondary damage. A 2024 study found athletes who maintained rehab exercises for 6+ months had 33% fewer knee injuries than those who stopped after clearance.
Always consult your care team before increasing intensity. Small adjustments preserve ligament health while adapting to lifestyle changes. Consistent care keeps the knee joint functioning optimally through decades of activity.
